A fistula in general is a connecting duct in the tissue that is not part of normal development. Fistulas can form in different areas of the body. In some cases, they are already present at birth (e.g. in the case of anal atresia), but mostly they develop in the course of life as a result of other diseases.
Anal fistulas occur at the proctodeal glands (apocrine sweat glands) in the anal canal and lead outwards to the skin. They permanently release secretions and, if large enough, also stool, which is why they can often lead to extremely unpleasant discomfort.
The risk of developing anal fistula is 1 to 3 percent, which means that 1-3 out of 100 people will develop an anal fistula in their lifetime. Men are affected more often than women. It is a relatively common condition in young men between the ages of 30 and 50.
The cause for the development of an anal fistula is often an anal abscess. Anal fistulas and anal abscesses have some things in common. An anal abscess is caused by bacteria. Here, purulent secretion accumulates in a capsule at the anal canal. If this inflammation becomes chronic, ducts can form and an anal fistula develops.
Other causes of an anal fistula can be:
Anal fissures are small tears in the anal area. If an inflammation forms as a result of this, it can develop into a fistula.
Haemorrhoids are protrusions of the mucous membrane in the area of the mucous membrane of the anus. Fistulas can also form here, especially in the case of infections.
Also chronic inflammatory bowel diseases such as ulcerative colitis or Crohn's disease can lead to the formation of fistulas. This is more common in Crohn's disease, but here the fistulas form in the entire gastrointestinal tract from the mouth to the anus. In ulcerative colitis, the risk of fistula formation is lower, but limited to the rectum.
Malignant diseases of the rectum (rectal carcinoma and anal carcinoma) can also lead to the formation of anal fistulas, although here too this is usually the result of an accompanying infection.
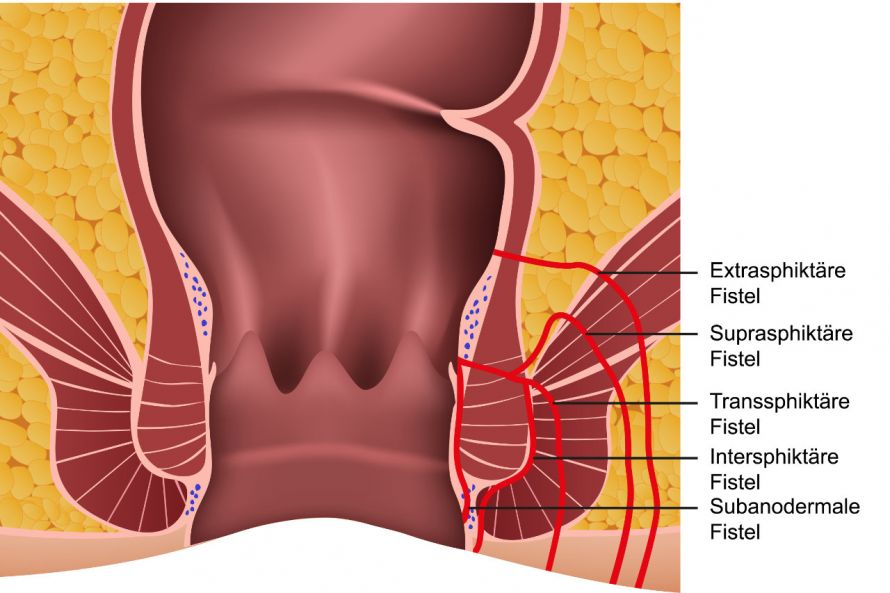
Decisive for whether a fistula is visible from the outside is its distance from the skin of the anus, the course through the sphincter muscles and its depth.
There are five different types of anal fistula, depending on their shape and course.
The basis of the classification are:
- the distance between the fistula opening and the anus (bowel outlet) and
- whether one or both sphincter muscles (medical term: sphincter ani) are affected.
There is an external sphincter (M. sphincter ani externus) and an internal sphincter (M. sphincter ani internus), which are both located next to each other and are responsible for the control of bowel movements (continence). The external sphincter in particular is of great importance here, as it is controlled voluntarily.
The classification of anal fistulas according to the distance to the anus is as follows (the distance increases from top to bottom):
- submucosal (runs directly under the mucosa, not through the muscles, opens into the anus)
- intersphincteric (runs between both muscles, opens close to the anus)
- transsphincteric (runs through both muscles)
- suprasphincteric (runs through the internal and above the external sphincter)
- extrasphincteric (runs above both sphincters)
The first three types occur frequently, whereas the last two forms of anal fistula are rare.
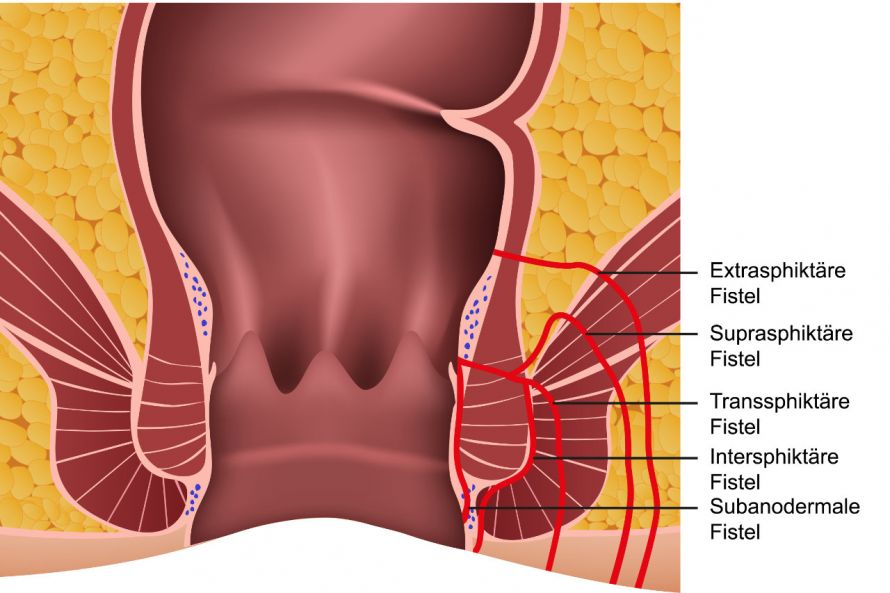
Illustration of different anal fistula shapes and their progressions © bilderzwerg | AdobeStock
Affected people initially either do not notice the fistula at all or it appears as a kind of pimple in the anal area. This supposed pimple can swell, itch or cause pain. In addition, purulent discharges may occur.
These symptoms can also occur with an abscess. In addition, general feelings of illness such as fever or a feeling of general malaise can also develop. When the fistula has formed, these complaints have usually already improved. This is because pus can drain through the fistula and the pressure is significantly reduced.
The following symptoms can occur with an anal fistula:
- Redness
- Swelling
- Itching,
- Pain,
- Purulent discharges, sometimes mixed with faeces
If a patient is suspected of having an anal fistula, it is advisable to see a specialist in rectal diseases, a proctologist.
During the examination, the anal area is first palpated. In addition, a rigid metal tube with a light source at the end (medically called a proctoscope) is often inserted. This allows the walls of the anal canal to be assessed so that, in addition to anal fistulas, also
can be identified.
Since an anal fistula can also be caused by a malignant tumour, tissue samples should be taken from suspicious findings and then examined histologically.
A fistula probe is used to determine the progression of a fistula. This is a metal tube that is carefully inserted into the fistula tract from the outside and can ideally be visualised on the inside with the proctoscope.
Most uncomplicated fistulas can be diagnosed with this. In the case of complex or multiple (several) fistulas and the suspicion of abscesses, additional ultrasound examinations and an MRI are also helpful in determining any damage to the anal area.
In many cases, an anal fistula must be treated surgically, as it rarely heals on its own.
In surgical treatment, the fistula is split. However, depending on the progression of the fistula, there is also a risk of injury to the sphincter muscle. This can be cut or severed during removal. Since the external sphincter muscle in particular is important for conscious control of bowel movements, its severance should be avoided if possible. The risk or need for partial or complete damage to the external sphincter is greatest with supra- and extrasphincteric fistulas. Fortunately, these make up only a small proportion of fistulas.
Nevertheless, in extreme cases, the function of the muscle may be restricted. The consequence is possible incontinence. To avoid this, the sphincter can also be sewn back together after the split fistula has healed.
Alternatively, the fistula can be closed with plastic and sutured shut. With this method, however, the risk of an anal fistula occurring again is higher.
Patients suffering from chronic bowel diseases cannot always be operated on. In addition, they are sometimes at risk of developing an anal fistula more often or again. They then either have to live with these fistulas or find relief by administering other medicines. Fistula drainage may also be indicated here.
If the anal fistulae are completely removed, the prognosis is good to very good. However, the healing process can often take several weeks and can sometimes be very painful. It is particularly important that patients ensure adequate anal hygiene – especially after surgical procedures. However, the preventive effect of good anal hygiene should also be emphasised at this point, especially as this can prevent anal fistulas or inhibit their growth.
However, if the fistulas cannot be completely removed, problems can still occur. People who suffer from Crohn's disease or other intestinal diseases have a particularly high risk of developing anal fistulas.