Osteochondrosis in the spine is a gradual disease that the affected person does not even notice at first. At first, pain occurs sporadically. Later, the back also hurts when lying or sitting, so that the suffering of those affected is great.
Intervertebral osteochondrosis is a change in the vertebral joints, intervertebral discs, and vertebrae in the cervical, thoracic, and/or lumbar spine. As a result, there can theoretically be greater wear on these structures; the medical profession refers to this as degeneration.
The causes of this type of osteochondrosis of the spine are not yet fully understood. Local circulatory disturbances in the bone, growth changes, or long-term overloading or incorrect loading of the back may play a role. Osteochondrosis can also develop as a result of intervertebral disc changes.
Osteochondrosis of the spine can cause pain, which can also worsen over time. Patients then often adopt a relieving posture due to the pain in order to relieve the affected structures. However, smaller osteochondroses may remain asymptomatic and are sometimes discovered as incidental findings, e.g., during an MRI examination. As a rule, this is no cause for alarm.
Possible symptoms of a pronounced disease are:
Back and neck pain are common with extensive osteochondrosis of the spine. Headaches and movement restrictions are possible accompanying symptoms. In some cases, pain can also radiate. If the disease is very advanced, physicians speak of erosive (advanced) osteochondrosis. If several joints are affected at the same time, this is called multisegmental osteochondrosis.
Osteochondrosis has many faces. The most common form is intervertebral osteochondrosis. This is a change in the vertebral joints, intervertebral discs, and vertebrae of the spine. If this is accompanied by signs of wear and tear, it is often also referred to as a spondylosis.
Spondylosis is non-specific wear and tear in the area of the spine. This leads to overloading the affected joint, and the bone is slowly broken down. The body counteracts wear by producing bone mass. However, this results in ossification of the affected segment. The transition from the lumbar spine to the pelvis (L5/S1) is most frequently affected.
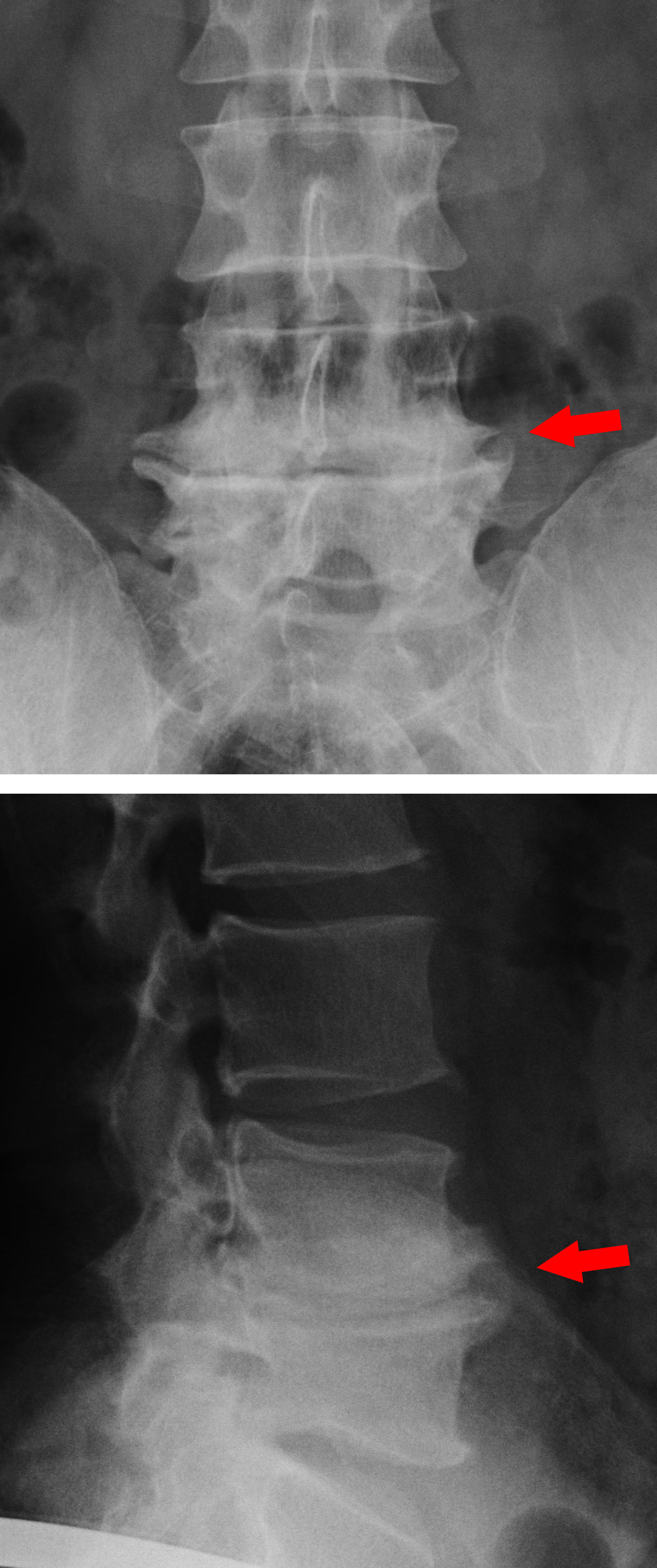
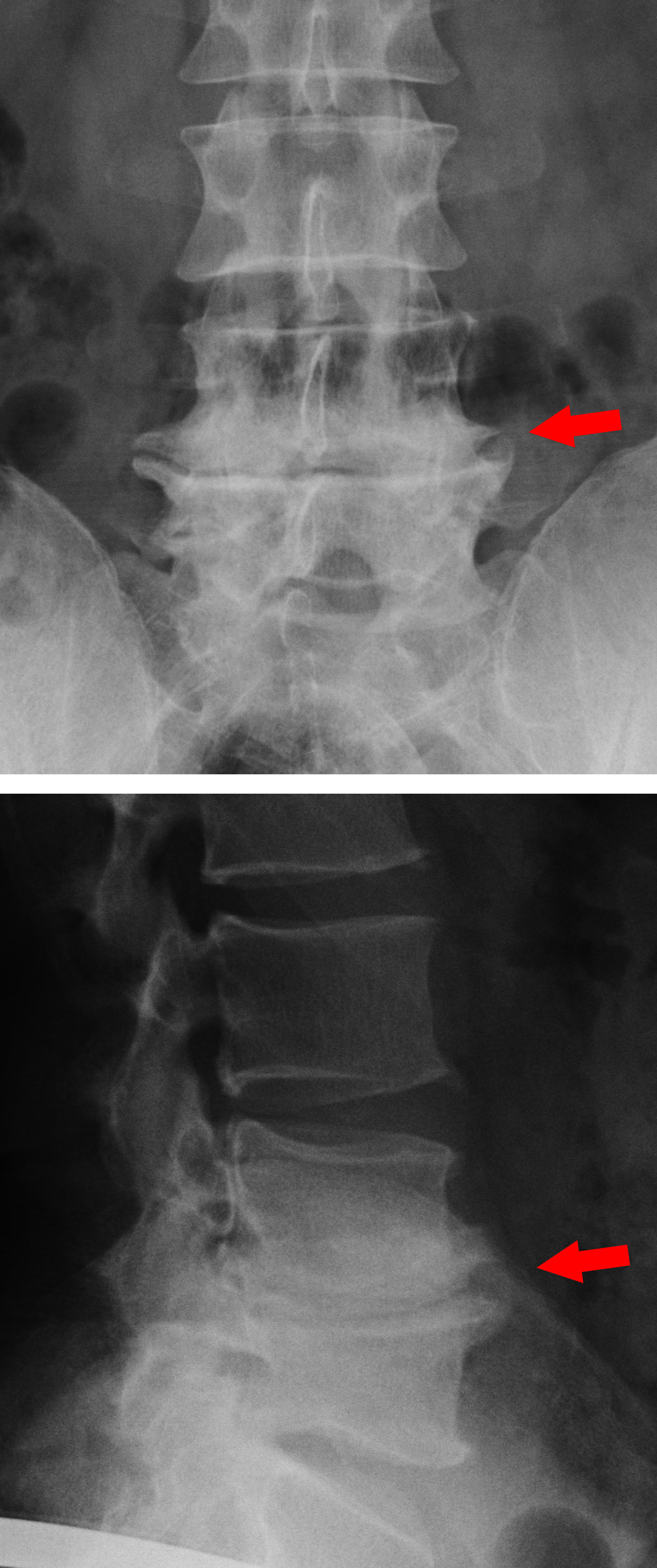
Osteochondrosis between the fourth and fifth lumbar vertebra; By Dr. Jochen Lengerke - Practice Dr. Jochen Lengerke, CC BY-SA 3.0 de, Link
Other forms of the disease:
1. Osteochondritis dissecans (activated osteochondrosis)
This is a change in bone metabolism with the involvement of the articular cartilage. This condition occurs mainly in the ankle, knee, or elbow joints. In a late stage, the cartilage-bone fragment is rejected into the joint, which can lead to painful signs of impingement there.
2. Scheuermann's disease (juvenile osteochondrosis)
Scheuermann's disease is a growth disorder of the thoracic spine and is the most common spinal disease in adolescents. In most cases, the changes begin between the ages of 11 and 13, and boys are affected more often than girls. The actual cause of this disease is not yet fully understood. In addition to a hereditary component, one-sided stresses on the spine, and poor posture due to weak core muscles contribute significantly to the development of Scheuermann's disease.
3. Legg-Calve-Perthes disease
Legg-Calve-Perthes disease is an osteochondrosis in the region of the femoral head, which occurs between the ages of 5 and 9. Children complain of pain in the hip or in the knee, which is caused by the changes in the femoral head and the joint effusion that occurs. If left untreated, Legg-Calve-Perthes disease can lead to permanent deformities of the femoral head after growth completion. During growth, the disease can often be cured by targeted surgical procedures.
Most patients come to the office with acute or chronic pain. The medical history, the medical clinical examination, and the analysis of the posture and gait pattern are the basis of the diagnosis. Nevertheless, the physician will perform complementary imaging to confirm the diagnosis. Various X-rays, magnetic resonance imaging (MRI), and ultrasound exams help determine the severity of osteochondrosis.
First and foremost, the therapy depends on the patient's clinical picture and the stage of the disease. The basis of non-surgical (conservative) therapy is painkillers and exercise therapy. Painkillers (analgesics) not only relieve pain, they are also helpful for relieving muscle tension. Sometimes additional inflammation occurs in the affected regions, which is why the doctor administers anti-inflammatory drugs.
As an adjunctive therapy, physiotherapy treatments help to relieve pain and improve mobility. Physical measures such as magnetic therapy, oxygen therapy, electrotherapy, heat treatments (fango or mud packs), or massages have no relevant influence on bone metabolism and cannot heal the disease. At most, such procedures should be used as adjunctive therapy, e.g., to relax the muscles. Scientific studies have also shown that relieving the strain (e.g., on forearm crutches) also shows no lasting benefit.
Sports are recommended in osteochondrosis with muscular weakness to stabilize the muscles around the joint. However, make sure that the type of sport does not put additional stress on your joints. Sports that are gentle on the joints, especially
- Swimming,
- Nordic Walking, and
- Cycling
are ideal in this respect. Also, make sure you eat a nutritious, Mediterranean diet.
Osteochondrosis can occur throughout the skeleton of the body but the spine is commonly affected. The treatment for osteochondrosis depends on the affected joint and the stage of the disease. In addition to conservative therapy, there are successful orthopedic surgical treatment procedures to alleviate the condition and prevent possible secondary damage.