Recommended specialists
Article overview
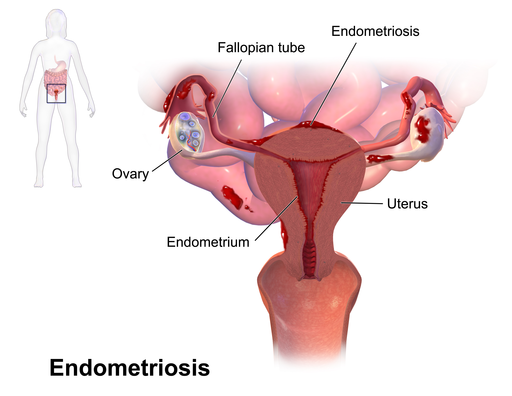
Endometriosis affects over 10 million women worldwide. It is most common in women who are in their thirties and forties. However, in rare cases, it can also occur in young girls.
Causes of endometriosis
Your body rids itself of the uterus lining during a regular menstrual cycle. Menstrual blood then flows from the uterus, through the cervical opening and out through your vagina.
However, a form of endometriosis known as retrograde menstruation can occur if, instead of flowing out of your body, menstrual blood actually flows back through your fallopian tubes and thus into the region of the pelvic cavity. During this process, endometrial cells can cling to any of the surfaces they encounter – such as pelvic walls and organs such as the ovaries, bladder and rectum. Once in position, they grow, thicken, break down and bleed during the menstrual cycle. Menstrual blood can also gain access to the pelvic cavity via a surgical scar.
Though it’s not clear why this happens, the disorder may also occur if small sections of abdominal tissue transform into endometrial tissue. It has been suggested some abdominal cells that form from embryonic cells may mutate and then behave like endometrial cells.
Symptoms of endometriosis
Endometriosis can present various mild, moderate or severe symptoms. The degree of pain experienced is not necessarily related to the extent of the condition – for instance, some women may have an acute form of the disorder and yet report fairly mild discomfort.
Pain in the pelvic region is the most typical symptom of endometriosis. However, there may be other symptoms too, such as:
- acutely painful menstrual cramps
- lower back pain just before beginning a menstrual period
- experiencing pain during sexual intercourse
- vaginal bleeding after sexual intercourse
- abdominal swelling
- fever
- a general feeling of sickness
- rectal pain
- experiencing pain during bowel movements
- constipation
- infertility (which for some women may be the only indication they have endometriosis. Endometriosis accounts for up to 40% of female infertility.)
- abnormal bleeding before the start of a menstrual period
- blood in the stools or in the urine
Though you may experience none of these symptoms, an annual gynaecological examination will be required to check for any changes.
Diagnosis of endometriosis
Painful or heavy periods can have many causes, so your doctor will conduct the following tests to reach an accurate diagnosis:
- a medical history and physical examination to note your symptoms as well as your general health, and to check for any family history of endometriosis
- ultrasound may be used to create an image of your reproductive organs to check for cysts that are linked with endometrial disorders
- a laparoscopy (a minor surgical procedure) may be called upon to confirm a diagnosis of endometriosis
Treatment of endometriosis
Endometriosis cannot be cured, but both medical and surgical options can offer relief from its symptoms. The chosen response will usually be in line with the degree of severity of your condition, and may include some of the following treatments:
- supplemental hormonal therapy can sometimes address the problem of abnormal tissue growth
- hormonal contraceptive measures (e.g. birth control pills) may also address endometrial tissue growth and reduce pain
- gonadotropin-releasing hormone (Gn-RH) agonists and antagonists can act to prevent menstruation, but may have side effects that mirror menopausal symptoms
- danazol is also employed to halt menstruation, though this medication may produce side effects
Common pain medication (e.g. ibuprofen) can sometimes alleviate the pain caused by endometriosis. However, other options are available:
- pain clinics can offer specialised pain-management support for those in chronic pain
- transcutaneous electrical nerve stimulator (TENS) machines, which prompt the body to produce its own pain-reducing endorphins, can offer an alternative approach to medication
- physiotherapy can offer exercises and relaxation techniques to strengthen the pelvic area, provide some pain relief and overcome stress and anxiety.
If surgery is considered necessary, this may take the following forms:
- conservative surgery, which aims to preserve your reproductive organs while reducing abnormal tissue growth via minimally invasive laparoscopy, or else via more traditional abdominal surgery
- radical hysterectomy is a final solution if nothing else helps, though it is always advisable to seek a second opinion – especially for women in their childbearing years, who will no longer be able to become pregnant
Some forms of endometriosis may have complex features, perhaps requiring the assistance of a number of different experts and specialisms, including:
- advanced laparoscopic surgery to confirm a diagnosis
- pain management strategies to cope with a range of painful symptoms
- a reproductive endocrinologist to assess and advise on fertility issues
- a gynaecologist surgeon to perform a detailed surgical intervention
Chances of recovery from endometriosis
Not all therapy and interventions will work for all women, and some may have a recurrence of symptoms after surgery or pseudo-menopause treatments. In the majority of cases, treatment will offer significant relief from pelvic pain. Infertility treatment may perhaps be an option for women with endometriosis who are finding it difficult to conceive. Besides fertility drugs, many find IVF (in-vitro fertilization) procedures to be effective.
Prevention of endometriosis
Endometriosis cannot be prevented. The fact that this disorder is poorly understood is a contributing factor, though long-term treatment with birth-control hormones has often been shown to help prevent the condition from getting worse.
Finding qualified endometriosis specialists
Doctors and surgeons who offer endometriosis treatment are best judged by their track record. Relevant factors will include the number of years they have practised as an endometriosis specialist, details of successful outcomes, as well as evidence of membership of leading societies or professional bodies and participation in endometriosis research.
All medical experts presented on this page are carefully selected and meet our strict admission criteria.