A retinal detachment occurs when the retina separates from the choroid inside of the eye. Fluid collects between the layers at the back of the eye, and the retina bulges into the eyeball like a bubble. At this point, the retina cannot be supplied with oxygen and nutrients from the choroid.
This can result in functional disorders, ranging from a loss of visual field to complete blindness. However, if treated early, the vision of the affected eye can usually be saved.

A retinal detachment in the light of a slit lamp
Retinal detachment affects one in every 10,000 people, or 0.01% of people. In addition to nearsightedness, risk factors include previous cataract operations, diabetes mellitus, and inflammation or tumors in the eye.
Depending on the cause, eye doctors differentiate between rhegmatogenous, exudative, and tractional retinal detachment, the three different forms of the condition.
Rhegmatogenous Retinal Detachment
If the retinal detachment occurs because of the tearing of the retina, it is considered a rhegmatogenous or tear-related detachment. It is most likely caused by a shrinking of the vitreous body that comes with aging. The vitreous body, consisting of a gelatinous mass, is located inside of the eyeball.
As a result of the shrinking, the vitreous body “pulls” on the retina so that it tears. This creates holes where liquid can escape from the vitreous body. The liquid then seeps between the retina and the underlying pigment epithelium which leads to the retina detaching.
The main risk factor for a rhegmatogenous retinal detachment is the age of the patient. Risks also include:

Older people in particular are at increased risk of retinal detachment due to tears © Wira SHK / AdobeStock
Tractive Retinal Detachment
Retinal detachment is caused by traction or tension that occurs when tissues of the retinal body and/or layers of the retina scar. The area around the scar is then shortened, creating a pulling effect. In many cases, diabetic retinopathy ‒ i.e. a damaged retina caused by long-term diabetes‒ triggers tractive retinal detachment. However, it is sometimes a late-term consequence of premature retinopathy.
Tractive retinal detachment can often be seen in relatives, so the risk of this condition is higher for patients whose family members have also gotten it.
Exudative Retinal Detachment
This rarely-diagnosed form of retinal detachment is caused by fluid retention. In this form, fluid escapes from the vessels of the choroid and accumulates between the retina and the pigment epithelium.
This is commonly caused by inflammation or tumors within the eye. Inflammation can happen in conjunction with other serious diseases, such as AIDS. In tumors caused by conditions like choroidal melanoma, the newly formed vessels are “leaky” and fluid accumulates under the retina.

The structure of the human eye
Flashes of light, eye floaters, loss of visual field
Typical complaints of retinal detachment include flashes of light, spots, lines, and blurry patches. In addition, some patients also report “soot flakes,” i.e., what looks like a swarm of black dots.
Other people may see a disturbing dark curtain or shadow in their vision because in areas of retinal detachment light cannot be perceived. This results in a loss of visual field, which is perceived by the patient as a dark curtain or veil.
If you experience any of these symptoms, you should consult an ophthalmologist immediately!
Eye Floaters
So called “eye floaters” are usually harmless, and they are caused by opacities of the vitreous body. They appear as almost transparent dots or streaks, and they commonly appear in front of light backgrounds or while reading.
Be advised: if you notice floaters for the first time or notice a change in them, you should consult an eye doctor as a preventative measure if only to rule out a retinal tear and the risk for retinal detachment.

„Eye floaters“
An eye doctor will make the diagnosis by examining the back of the eye. If they only observe flaws in the retina, these can be treated with a laser. However, if the retina has already peeled off, only surgery will usually help. Retinal holes, like retinal detachment, cannot be treated with medication.
The doctor will usually examine both eyes, even if the patient only has symptoms in one, because there are often also changes in the apparently healthy eye. These often end up being precursors to retinal detachment. The doctor can then treat them preventatively with a laser.
Ophthalmoscopy & Co.
The actual eye examination is usually carried out with an ophthalmoscope, with the pupil having been dilated with medication. This procedure is necessary because the retina in the back of the eye cannot be seen with the naked eye.

Examination of the eyes by ophthalmoscopy © Henrik Dolle / AdobeStock
For this purpose, the patient is given eye drops in preparation for the operation that cause the pupil to dilate. Therefore, patients should not drive themselves alone to the examination, because the dilated pupils make it impossible to drive immediately afterwards.
With the help of a lightsource, an ophthalmologist will illuminate the ocular fundus in order to make a potential retinal detachment visible.
It is not uncommon for a magnifying glass-like aid to also be used by ophthalmologists to diagnose retinal detachment by placing it on the eyeball. Using this, the doctor can identify a retinal detachment and, in certain cases, its cause in the retina, such as a tear. If the retina is already detached, this is often seen in raised gray folds.
If bleeding in the vitreous body of the eye makes it impossible to see the retina, the doctor will perform an ultrasound examination instead. This is how changes in the retina can be identified.
Surgery is almost always necessary to treat retinal detachment. There are several surgical procedures for this. The two most important are
- Scleral buckle surgery
- Vitreous surgery (vitrectomy)
A laser can also be used to treat retinal detachment.
Laser Treatment
Retinal detachment and retinal tears cannot be treated with medication. In the event of a retinal tear ‒ i.e., before the onset of retinal detachment ‒ a laser can help the affected eye.
With the help of a laser beam, the doctor can cause an inflammatory reaction in the injured area. This results in the tissue becoming scarred and the holes in the retina sticking together. With this process, retinal detachment can be counteracted in many cases.
Eye Operation
If retinal detachment has been diagnosed, however, laser treatment is ineffective. In such cases, only eye surgery will help. The surgical methods depend largely upon the form and stage of the retinal detachment.
The focus of these procedures is on fixing the detached retina and eliminating the triggering factors, such as changes in the vitreous body.
Additional Forms of Treatment
If inflammation is the cause for the retinal detachment, treating the underlying condition is essential.
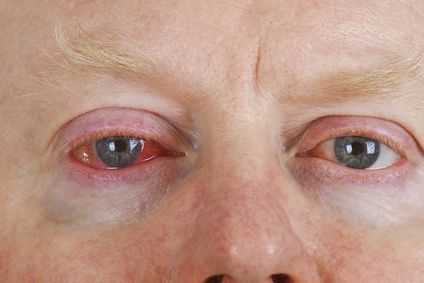
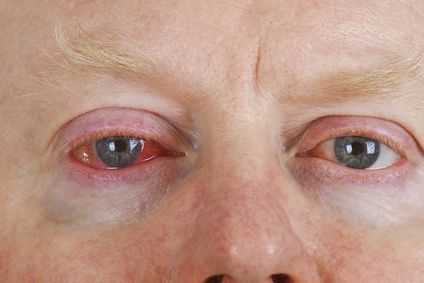
Eye inflammation can cause retinal detachment © Birgit Reitz-Hofmann / Fotolia
If tumors are instead responsible, a specialized center for tumors should be responsible for treatment. There are various treatment options, such as surgically removing the tumors or radiation. The latter treatment may necessitate irradiating the entire eyeball, or it can take place as local irradiation, by beaming radiation directly on the eye.
The following surgical procedures are available for the treatment of retinal detachment:
Scleral Buckle Surgery
If there is a single hole or tear, this surgery is used.
The surgeon sews a seal, usually made out of silicon rubber, onto the sclera from the outside. This causes the dermis to indent and the retina is brought to rest on this hump. The application of freeze treatment through a cryoprobe supports this cohesion. The surgeon then drains the liquid that has accumulated under the retina through a puncture from the outside.
A special type of this indenting operation is the application of a band that presses into the sclera, called a cerclage.

Retinal detachment almost always needs to be treated with surgery © DragonImages / AdobeStock
Belt Operation
If there are several holes, a belt operation can be carried out: the surgeon pulls a band around the entire eyeball and shortens it until a circular constriction occurs. A puncture in the area between the retina and choroid is used to remove fluid. The surgeon then seals the holes or tears using a seal or band.
Internal Eye Surgery
The two previously mentioned surgical methods do not always guarantee success. If the retinal detachment of the eye has been present for a long time and adhesions can already be recognized, there is no avoiding a so-called pars-plana-vitrectomy.
When the vitreous body has been removed from the eye, the adhesions are detached, or rather the strands of connective tissue are eliminated.
The surgeon then removes the vitreous: this can be done with a gas as well as with silicon oil. Both methods allow the retina to be pressed against the choroid from within.
In nine out of ten patients, eye surgery is successful after the first time; that is to say, retinal detachment can be cured with surgery. In some cases however, retinal detachment occurs again later. Another medical intervention is then unavoidable.
The treatment of retinal detachment places high demands upon the surgeon, and patients should be aware of this. For this reason, you should choose an eye center that specializes in this type of surgery.
Even after a successful retinal surgery, there is usually reduced visual acuity or visual field loss compared to the patient’s vision prior to their retinal detachment.
However, retinal detachment ultimately occurs depending on various factors, such as how far the retinal detachment has progressed, and how long the detachment existed before the operation.
This means that the progression and prognosis of a retinal detachment ‒ both for the eye and vision ‒ are all the better and more informative, and:
- The less retinal tissue is affected,
- The shorter the period of time of the retinal detachment, as well as
- The less complicated the initial finding is
Anyone who has had a retinal operation should refrain from physical exertion for at least the following few weeks, including exercising and lifting heavy objects. For the first few days afterwards, you should avoid anything that causes your eyes to move back and forth quickly. Above all, this includes reading. Television, however, (where your eyes are fixed in one direction) is allowed.
Eye checkups should be carried out every couple of weeks and then every couple of months.
If the symptoms previously mentioned, such as lightning, darkening, or deterioration of your vision reoccur, you should immediately consult an ophthalmologist or an eye clinic.

Regular ophthalmological checkups are necessary after the surgery © M.Dörr & M.Frommherz / AdobeStock
Symptom-related Examination
You should see an eye doctor immediately after the first signs of retinal detachment. If you notice flashes of light or the sudden appearance of black dots, an immediate visit to the ophthalmologist is mandatory. If your visual field is restricted, you can assume that your retina is already in the process of detaching.
Regular Examination
A regular examination of your eyes is generally advised if you are at an increased risk for retinal detachment. This is the case, for example, when:
- You have severe nearsightedness,
- You had a cataract surgery not long ago, or
- You have previously had a retinal detachment.
An eye examination also provides information about possible degenerations of your eye health that can lead to something worse.
Using lasers to treat such changes in the retina is a preventative measure. The scars that form later on the lasered area weld the retina to the choroid.
It should be expressly noted that this preventative measure is only possible as long as there is no retinal detachment present.