Since symptoms of hypothyroidism are very non-specific, the disease may remain undetected for a long time. The diagnosis is made based on a laboratory blood test.
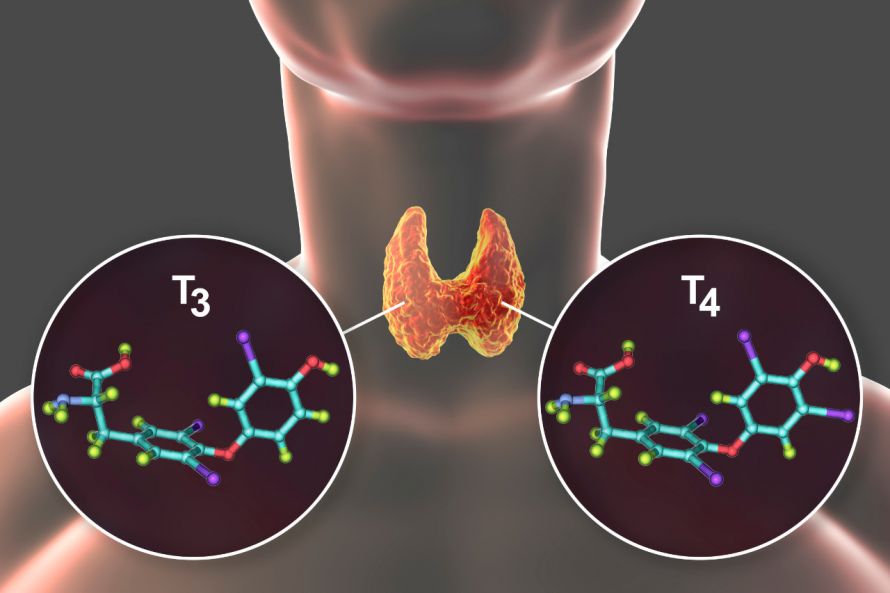
Manifest hypothyroidism is characterized by the deficiency of triiodothyronine and thyroxine (usually abbreviated as T3 and T4) described above.
In addition, there is also the so-called latent or subclinical hypothyroidism. Here, the body still manages to increase the levels of T3 and T4 into the normal range through increased stimulation of the thyroid gland. Latent hypothyroidism is usually asymptomatic but can develop into manifest hypothyroidism.
According to estimates, about five percent of the population in Germany is affected. Women are affected about five times more often than men.
The thyroid gland and a molecular depiction of the T3 and T4 hormones © Kateryna_Kon | AdobeStock
Hypothyroidism can be congenital or acquired.
Congenital hypothyroidism requires urgent treatment even in infancy. Otherwise, there is a risk of significant physical and mental developmental disorders.
Acquired primary hypothyroidism is the most common form of hypothyroidism. Here, the hormone deficiency is directly caused by the thyroid gland.
In contrast, very rare secondary hypothyroidism is triggered by pathological processes in the pituitary gland. These disorders reduce the production of the regulatory hormone TSH. The thyroid gland itself is not affected but is not sufficiently stimulated by TSH.
Possible causes of primary hypothyroidism include
- Autoimmune inflammatory processes that destroy thyroid tissue (e.g., Hashimoto's thyroiditis),
- Loss of thyroid tissue due to thyroid surgery, radioiodine therapy for thyroid diseases, or irradiation in the head and neck area,
- Pronounced iodine deficiency,
- Excessive iodine intake, and
- Possible selenium deficiency.
Taking certain medications can increase the likelihood of developing primary hypothyroidism. These include:
In connection with hypothyroidism, a greater number of the following symptoms usually occur:
- Constant fatigue,
- Listlessness,
- Depression,
- Concentration and memory disorders,
- Constantly feeling too cold,
- A body temperature that is too low,
- A slowed heartbeat,
- Edema (swelling of the face and limbs due to water retention in the tissues),
- Joint pain,
- Muscle weakness,
- Loss of appetite, constipation, and nausea,
- Noticeable weight gain,
- Dry, itchy skin,
- So-called myxedema, a doughy thickening of the skin,
- Brittle nails, hair loss, and
- Menstrual disorders in women, libido disorders, and reduced fertility.
The combination of symptoms from several symptom groups indicates hypothyroidism. However, false positive or negative (self-)diagnoses are easily made. Blood tests provide clarity.
Hypothyroidism may or may not be accompanied by abnormal changes in the thyroid gland:
- Enlarged thyroid gland (goiter), especially in cases of iodine deficiency and congenital hypothyroidism and
- Reduced size of the thyroid gland: in case of destruction of the thyroid gland, for example, due to autoimmune inflammatory processes

Constant fatigue is one of the symptoms that can occur with hypothyroidism © pix4U | AdobeStock
The diagnosis of hypothyroidism is made based on a laboratory blood test. The level of thyroid-stimulating hormone (TSH) and thyroxine (T4) levels are measured. Determining the level of triiodothyronine (T3) is also possible, but this is not usually done as it does not provide any additional information.
An elevated TSH level is crucial for the diagnosis, especially for the more prevalent primary hypothyroidism. The elevated TSH level represents the body's initial response to low T3 and T4 production.
In latent hypothyroidism, TSH elevation may still increase regulation of T3 and T4 levels into the normal range. Elevated TSH levels and T3 and T4 levels within the (lower) normal range are then measured.
Subnormal T4 levels in addition to elevated TSH levels are characteristic of manifest hypothyroidism. Free T4, abbreviated as fT4, is usually measured.
The most common cause of hypothyroidism is the disease Hashimoto’s thyroiditis. To detect it, the levels of thyroid antibodies are usually also measured (microsomal antibodies and thyroglobulin antibodies). Unlike in Graves' disease ("TRAb" antibodies), microsomal antibodies and thyroglobulin antibodies do not have a stimulatory effect. Instead, they gradually destroy thyroid tissue, resulting in hypothyroidism.
In the case of hypothyroidism, an ultrasound examination of the thyroid gland is usually also performed.
Regardless of its cause, manifest hypothyroidism is treated with thyroid hormones. Levothyroxine (L-thyroxine) and liothyronine, structurally identical to natural triiodothyronine (T3), are available as active ingredients.
Usually, the therapy is carried out with L-thyroxine. In order to find the individually correct dose and to keep side effects low, the dosages of drugs are gradually increased: Initially, a low dose is prescribed. After four weeks at the earliest, the TSH level is checked and the dose may be increased.
This procedure is repeated until the symptoms have improved significantly and the TSH level is within the normal range.
Combination drugs for hypothyroidism contain combinations of levothyroxine and liothyronine (T3 and T4). They are not prescribed as first-line medications in primary acquired hypothyroidism. Combinations of T3 and T4, however, may help some patients in whom L-thyroxine alone is not sufficiently effective.
Latent hypothyroidism can also be treated with L-thyroxine if symptoms are present.
Treating congenital or acquired hypothyroidism with thyroid hormones must usually be continued for life. Hypothyroidism is not curable.
However, with proper and regular medication, the prognosis is favorable: Most affected individuals can continue their lives without significant limitations in their health and quality of life. However, the medication must not be discontinued independently and abruptly.
To avoid a severe disruption of the hormonal balance, the dose should not be changed abruptly, but only gradually. After starting the medication or after changes in the L-thyroxine dose, the TSH level needs at least four weeks to reach its new equilibrium. After this period, the level is checked to determine whether it is now within the normal range or whether the dose needs to be adjusted.
If the TSH level is normal and the patient is symptom-free, the patient is initially monitored every six months and later every year.