The pancreas is a human glandular organ located transversely in the upper abdomen on the posterior abdominal wall. It is about 15 centimeters long and weighs 70 to 100 grams. The pancreas produces digestive enzymes (exocrine function) and hormones (endocrine function).

The location of the pancreas (bottom right) in the body © nerthuz | AdobeStock
The two most important functions of the pancreas include
- The release of more than 20 different enzymes necessary for digestion into the duodenum, and
- The release of the hormones insulin and glucagon, which are necessary for controlling blood glucose levels.
If the pancreas is inflamed, physicians speak of pancreatitis or inflammation of the pancreas. In this case, it is the exocrine function of the gland that is primarily affected.
In pancreatitis, two diseases can generally be distinguished from one another: acute pancreatitis and chronic pancreatitis.
In acute pancreatitis, there is a very painful and sudden inflammation of the pancreas that occurs once.
In more than 80% of cases, the progression is mild and self-limiting, and the disease heals without significant long-term complications. In contrast, the severe type with necrosis (dying tissue) is a potentially life-threatening disease. Patients must then be treated in an intensive care unit. Numerous complications can occur during such a progression.
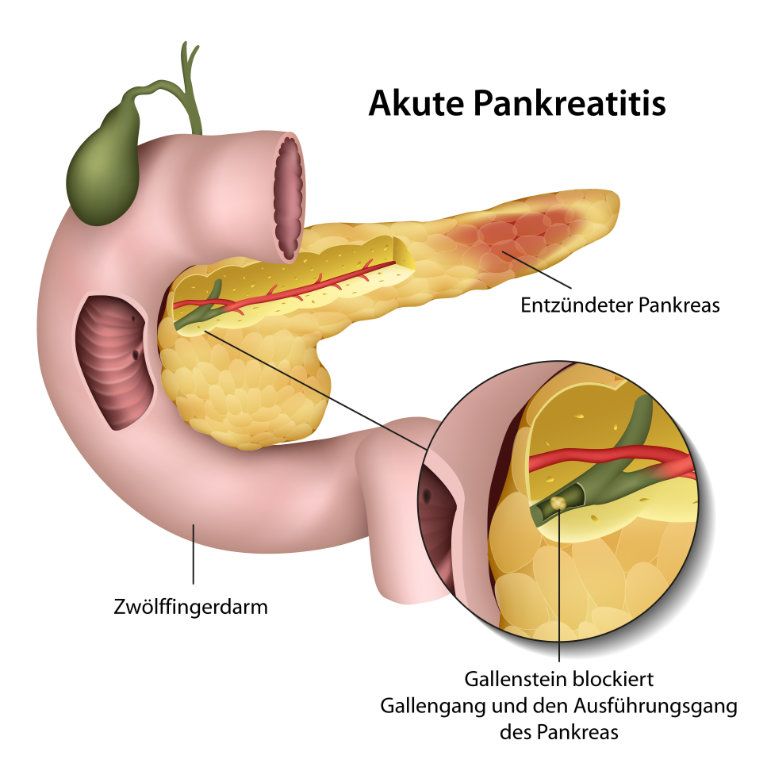
In acute pancreatitis, physicians distinguish between infectious and non-infectious pancreatitis. The decisive factor is the cause of the disease. Non-infectious causes of pancreatitis, such as excessive alcohol consumption and gallstones, are the most common triggers, accounting for 80% of all cases.
Possible causes of infectious pancreatitis include viruses (mumps or coxsackieviruses, etc.).
Chronic pancreatitis, on the other hand, occurs multiple times with acute episodes of pancreatitis and over a longer period of time. It leads to irreversible damage to the gland due to the increasing destruction of pancreatic tissue.
As a result, indigestion with fatty stools occurs due to the lack of enzymes in the diet. Due to the additional damage to the endocrine part of the pancreas, it also leads to pancreoprivic diabetes mellitus.
Pancreatitis is a disease that occurs very rarely. However, it has been increasing worldwide in recent decades. Acute pancreatitis affects between 10 and 20 people per 100,000 inhabitants in Germany and Central Europe every year. Women are affected slightly more often than men.
About 8-10 new cases of chronic pancreatitis occur per 100,000 inhabitants. Men are more frequently affected than women.
In childhood and adolescence, hereditary inflammation of the pancreas may also occur; this is then referred to as chronic hereditary pancreatitis.
Acute pancreatitis is caused by either migrating gallstones in the common bile duct or alcohol abuse in over 80 percent of cases. Other possible, but far less common causes of pancreatitis include
- Medication,
- Viral infections,
- Metabolic disorders,
- Hereditary factors,
- Malformations of the pancreatic ducts, and
- Damage to the pancreas due to injury or surgery.
In some rare cases, no cause can be determined; physicians then speak of idiopathic acute pancreatitis.
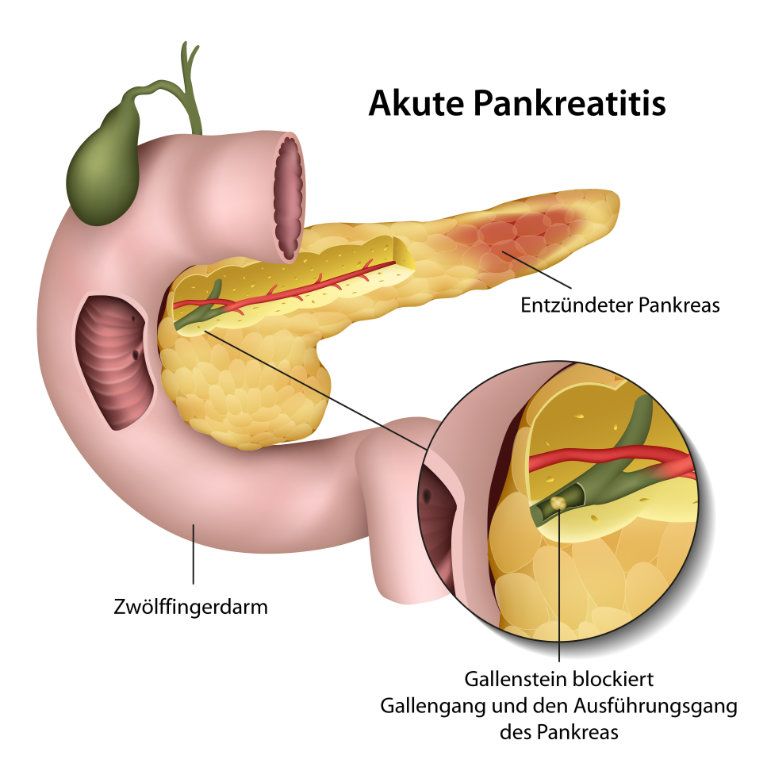
Pancreatitis can be caused by gallstones © bilderzwerg | AdobeStock
Chronic alcohol abuse is mainly responsible for chronic pancreatitis, along with the following factors in descending order of importance
- Heavy smoking,
- Metabolic disorders, and
- Mechanical factors (pancreatic duct obstructions due to, e.g., papillary tumors, etc.)
In rare situations, chronic pancreatitis can run in families and be inherited. In these cases, gene mutations in, for example, the digestive enzyme trypsinogen and the enzyme inhibitor SPINK1 are responsible. This causes the pancreatic juice to become prematurely active while still in the gland, resulting in a chronic inflammatory response.
The symptoms of pancreatitis vary depending on whether the disease is acute or chronic.
For example, acute pancreatitis is usually manifested by sudden, severe, belt-shaped upper abdominal pain that can radiate to the back or chest.
- Nausea,
- Vomiting,
- Flatulence,
- Constipation, and
- Fever
can also occur. In addition, there may be impaired bowel function up to and including bowel obstruction, shock, low blood pressure, and jaundice.
In principle, a distinction is made between two types of progression: Mild (80%) and severe (20%) acute pancreatitis.
Rapid clinical improvement is the result of appropriate therapy (abstinence from food and fluid replacement) and complete healing occurs in the mild type.
In the severe type, tissue death (necrosis) of the gland and the surrounding area occurs. This is referred to as acute necrotizing pancreatitis. Here, further deterioration of the condition with multiple organ failure can occur rapidly. In this case, intensive care with artificial respiration, circulatory support with catecholamines, and dialysis, etc. is necessary. It is therefore a life-threatening disease.
Therefore, it always requires treatment in the hospital as soon as possible. Depending on the degree of severity, an early, interdisciplinary treatment adapted to the individual can be carried out.
Chronic pancreatitis typically results in recurrent or persistent upper abdominal pain that may radiate in a belt-like shape to the back. It may be associated with nausea and vomiting. Due to the alterations in the connective tissue of the pancreas resulting from the destruction of normal tissue, digestive problems occur. This is accompanied by
- Flatulence,
- Diarrhea, and
- Fatty stools when eating fatty foods (exocrine pancreatic insufficiency).
As a result, weight loss occurs.
The damaged pancreas is no longer able to produce the hormone insulin, which regulates blood sugar. Therefore, about one-third of those affected develop diabetes mellitus as a result of chronic pancreatitis. This is referred to as pancreoprivic diabetes mellitus since the counter-regulating hormone glucagon is also no longer produced.
To diagnose acute pancreatitis, the physician first asks the patient about their medical history during an anamnesis interview. This is followed by a physical exam. If the patient reports symptoms typical of pancreatitis as well as gallstone disease or excessive alcohol consumption, this already provides the physician with a suspected diagnosis of pancreatitis.
A blood test is then performed to confirm the diagnosis. Among other things, the levels of the pancreatic enzymes amylase and/or lipase in the blood are measured.
With this triad (typical medical history, symptoms, and laboratory testing), "acute pancreatitis" can be diagnosed.
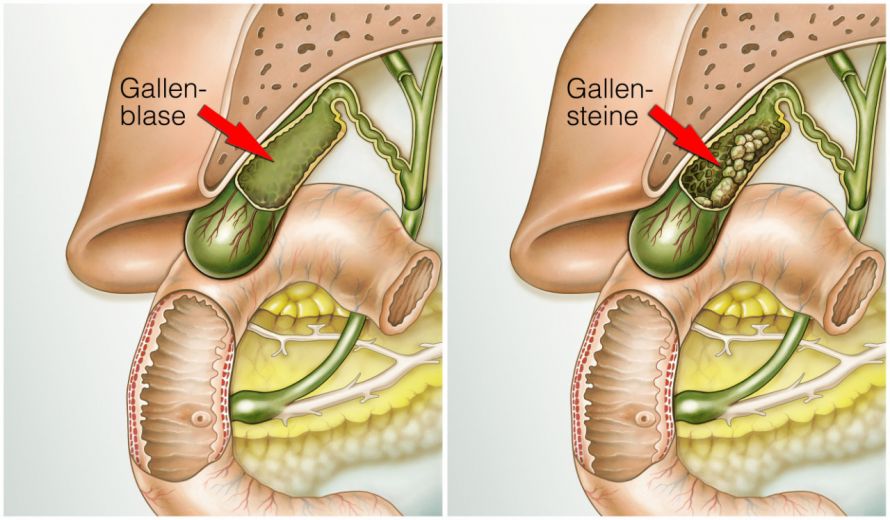
Since patients come to doctors and hospitals with acute symptoms, an ultrasound of the abdomen is generally performed. This allows, for example, gallstones to be found, corroborating the cause of gallstone-related acute pancreatitis. Since the pancreas is located in the posterior abdominal cavity and the abdomen is often distended, an accurate assessment of the inflammation at the pancreas cannot be performed with an ultrasound.
Subsequently, however, it is important to correctly assess the severity of the disease and thus its course. The distinction between mild and severe acute pancreatitis is made by means of
- Determining the inflammation value and the C-reactive protein (CRP) and
- A contrast-enhanced computed tomography (CT) scan.
Nowadays, the following imaging techniques are used to diagnose chronic pancreatitis
These can be used to visualize calcifications as typical signs of chronic pancreatitis and ductal changes (e.g., stones in the pancreatic duct and ductal dilatation).
In addition, there is a special endoscopic examination of the pancreatic duct and bile ducts. It is referred to as an ERCP. This is an invasive procedure that has a particular risk of triggering pancreatitis and is therefore used in a targeted manner nowadays. If indicated, gallstones can be removed from the pancreatic and biliary ducts. If jaundice is present, a stent is inserted to drain the bile.
In the case of a calcified pancreatic head tumor in chronic pancreatitis, a malignant tumor cannot be ruled out with absolute certainty. This can occur in up to 5% of cases with this disease.
In addition checking for changes to these organ structures and ducts, the exocrine and endocrine function of the pancreas is also examined. The general digestive performance is checked by determining the level of elastase in the stool.
- Measurement of the fasting blood glucose and the daily blood glucose profile,
- An oral glucose tolerance test, and
- The long-term blood glucose level (HbA1c)
can be used to regulate the endocrine of blood glucose.
Acute pancreatitis can be life-threatening if severe. Therefore, treatment is always provided at a hospital. A mild course can be treated in a general ward. Patients with severe acute pancreatitis, on the other hand, require intensive care in an intensive care unit.
Acute pancreatitis is treated by abstaining from food and the administration of enough fluids and painkillers. With these basic therapeutic measures, mild pancreatitis heals rapidly and the patient can quickly resume eating.
After that, it is then necessary to determine the exact underlying cause. In the case of gallstone-related pancreatitis, the gallbladder should be removed during the process, this is usually successful with a minimally invasive method.
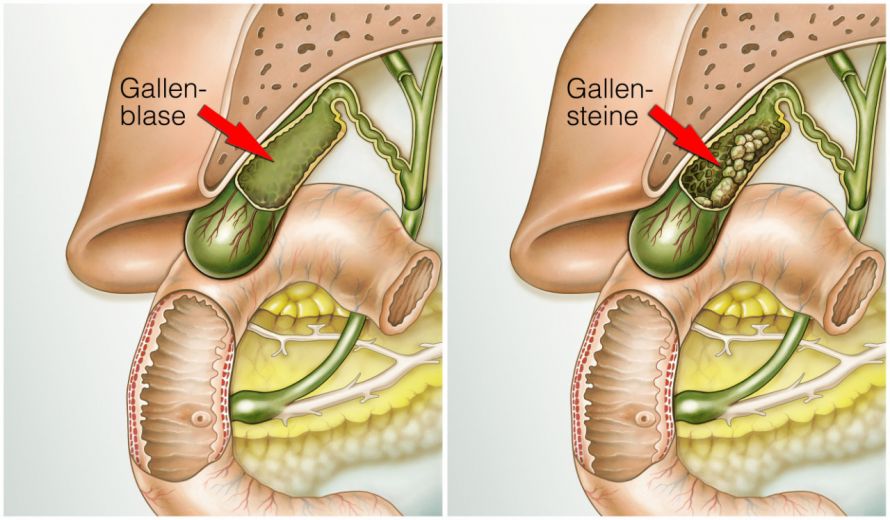
The gallbladder above the pancreas, with gallstones on the right © Henrie | AdobeStock
In severe acute pancreatitis, the digestive juice damages the gland and the area surrounding the pancreas. This is referred to as acute necrotizing pancreatitis. In this case, the initial focus of intensive care is treating its effects on the other organs: lungs, kidney, and heart.
It is not uncommon for these patients to require artificial respiration, dialysis, and medication to support their circulation. A so-called “step-up approach" is applied to the developing areas of necrosis if organ insufficiencies continue to persist. This means that less invasive measures are performed first and more invasive measures are considered only when needed.
Patients with severe acute pancreatitis should therefore be treated in specialized hospitals. Here, techniques such as inserting large-lumen drains with irrigation and performing necrosectomies via the stomach (transgastric necrosectomy) come into play.
If all this fails, minimally invasive and open necrosectomies are performed. This means that the best individual treatment concept must be applied on an interdisciplinary basis and depending on the extent of the disease.
In contrast to the past, pancreatic surgeons are required significantly less in acute pancreatitis. However, one can imagine that these patients often have a very long intensive care and hospital stay.
The severe course is still associated with a high mortality of 10-20% despite all the good measures.
An acute episode of chronic pancreatitis, which is usually mild, is treated similarly to acute pancreatitis.
In chronic pancreatitis, the patient must first avoid the causes leading to the disease. As a rule, this means permanently abstaining from the consumption of alcohol and nicotine. Pain is treated according to an adapted pain concept. Exocrine pancreatic insufficiency must be treated with enzyme capsules. In the case of endocrine insufficiency with the onset of pancreoprivic diabetes mellitus (diabetes mellitus type 3c), insulin is administered.

If diabetes develops as a result of pancreatitis, insulin therapy is necessary © Sherry Young | AdobeStock
Due to the chronic course of this type of the disease, increasing problems develop. It has been shown that early surgical intervention can favorably influence the disease’s progression. Therefore, pancreatic surgeons should be involved at an early stage on an interdisciplinary basis. This has been included as an important recommendation in the current guideline for the treatment of chronic pancreatitis.
A number of procedures are available for surgical treatment, each adapted to the specific patient case, including
- Segment resection,
- Pancreatic head resection that preserves the duodenum,
- The Whipple procedure, and others.
Mild acute pancreatitis usually does not result in complications or long-term damage. With the right therapy, it usually heals completely in very little time. So the prognosis is favorable. However, in the case of gallstone-related acute pancreatitis, the gallbladder should definitely be removed by laparoscopic surgery during the process.
The severe type with necrosis is still a life-threatening disease. Despite all the tiered maximum care measures, mortality is unfortunately 10-20%!
If this disease is overcome, only partial recovery often occurs and further interventions up to surgical intervention are required. In most cases, this type requires lifelong follow-up care and medical supervision by a gastroenterologist and in specialized centers.
Chronic pancreatitis is characterized by irreversible damage to the pancreatic tissue. In addition to chronic pain, tissue loss results in exocrine and endocrine pancreatic insufficiency. Due to the inflammation, local complications may also arise in the neighboring organs.
Surgical intervention can mitigate disease progression and damage to neighboring organs and structures. Again, as in acute necrotizing pancreatitis, lifelong medical supervision is necessary. The prognosis is good if the treatment measures are strictly based on the individual case and are optimally carried out. Early mortalities shall not be lamented.
However, the possibility of a malignant tumor developing should always be considered in chronic pancreatitis.