Recommended specialists
Article overview
Pancreatic surgery - Further information
Overview of pancreas surgery
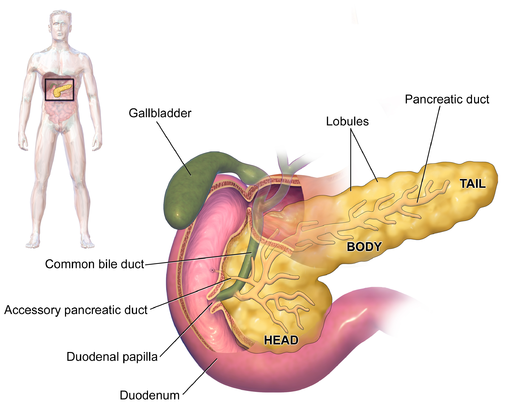
The pancreas is a large gland located behind the stomach, close to the small intestine, and is an important part of the body’s digestive system. Pancreas surgery is often termed a pancreatectomy – a surgical intervention to remove all or part of the pancreas. Several types of pancreatectomy can be performed, including pancreaticoduodenectomy (also known as a Whipple procedure), distal pancreatectomy, segmental pancreatectomy and total pancreatectomy. Each of these procedures can be employed to manage a number of conditions associated with the pancreas, for example, benign pancreatic tumours, malignant pancreatic cancer and pancreatitis.
Who offers pancreas surgery?
Pancreas surgery is commonly offered by specialist private health clinics, which are in some cases managed by universities, insurers, mutual societies or religious institutions. In addition, there are state-run hospitals (such as those managed by the UK’s NHS), which also employ skilled surgeons who specialise in various kinds of pancreas surgery.
What does pancreas surgery help with?
Pancreas surgery can help in the treatment of the following conditions:
- pancreatic cancer is often treated by a pancreatectomy to remove all, or a section of the pancreas. This abdominal organ consists of three sections – the head, the body and the tail – and the stage and growth of the cancer present usually dictates which of three types of surgical procedure are carried out. A pancreaticoduodenectomy is the most common intervention and removes just a portion of the pancreas, a distal pancreatectomy takes away the body and the tail, while a total pancreatectomy is used to take out the whole organ.
- a trauma or injury to the pancreas may result in a partial pancreatectomy. Even though this procedure removes otherwise healthy pancreatic tissue, the pancreas is still usually able to maintain its normal functioning, without any adverse effects.
- chronic pancreatitis – severe and continuing inflammation of the pancreas – is a painful condition that can also be treated via a pancreatectomy.
- severe hyperinsulinemic hypoglycaemia, a condition that results in low blood glucose levels due to excess amounts of insulin, can also be treated by pancreas surgery
When is pancreas surgery used?
Pancreas surgery is used when it is necessary to remove the pancreas (or partially remove it) to treat a number of conditions. The pancreatectomy procedure uses two different techniques:
- an open pancreatectomy requires one large incision to allow unrestricted surgical access to the pancreas
- a laparoscopic pancreatectomy is a less-invasive surgical procedure that requires four small incisions, a tiny surgical camera and some micro-surgical instruments to perform the internal operation
The surgical methods used during a pancreatectomy will be selected according to the precise extent of the planned surgery. For instance:
- in a partial (or segmental) pancreatectomy the pancreas is simply stapled firmly in order to allow the extraction of the section that is to be removed – sometimes the spleen may also be taken away as part of the procedure
- during a total pancreatectomy, not only is the whole pancreas organ removed, but a new connection must be made to attach both the stomach and the bile duct to the small intestine
An important part of any pancreas surgery intervention is the attachment of a number of tubes to facilitate postoperative care arrangements. These would normally include:
- a temporary drain leading from the body to enable tissue fluids from the wound area to drain away and prevent any large volumes accumulating, which could otherwise cause problems
- a gastronomy tube (g-tube) connected to the stomach, which helps to prevent bouts of nausea and vomiting
- a jejunostomy tube (j-tube) can also be connected to the small intestine to provide a route for supplementary nutrition during recovery
What are the risks of pancreas surgery?
Some of the main risks and complications that can occur as a result of pancreas surgery include:
- excessive bleeding
- wound infections
- post-operative weight loss
- delayed gastric emptying (solids and liquids are slow to leave the stomach)
- pancreatic anastomotic leak (leakage from the point where the bowel is reconnected)
- fistula development (false channels joining the pancreas to the bowel)
- diabetes (as a result of removing too many insulin-producing cells during surgery)
Are there alternatives to pancreas surgery?
For conditions such as pancreatic cancer, both chemotherapy and radiotherapy treatments might be considered as possible alternatives to pancreas surgery. However, this would depend on many factors, such as the age of the person and the precise location and stage of growth of any cancerous cells present.
Dependent upon the medical condition involved, some patients may be considered suitable for a pancreas transplant.