The term “glaucoma” is derived from a greek word meaning something like shiny, bright, or shining. If used to describe the sea, the word means bluish. This name derives from the blue-gray color of the iris that occurs in chronic inflammation.
Prevalence of Glaucoma
Glaucoma is one of the leading causes of blindness worldwide. In Germany, around 500,000 people suffer from increased intraocular pressure or glaucoma. About ten percent of them are at risk of going blind as a result. However, the number of cases that go unreported is probably higher.
At a younger age, men and women have an equal likelihood of being affected by glaucoma. Acute glaucoma can occur in all ages, but the risk of getting it increases with age. Women are also more often affected than men.

Old age is a risk factor for the development of glaucoma
Anatomical Background
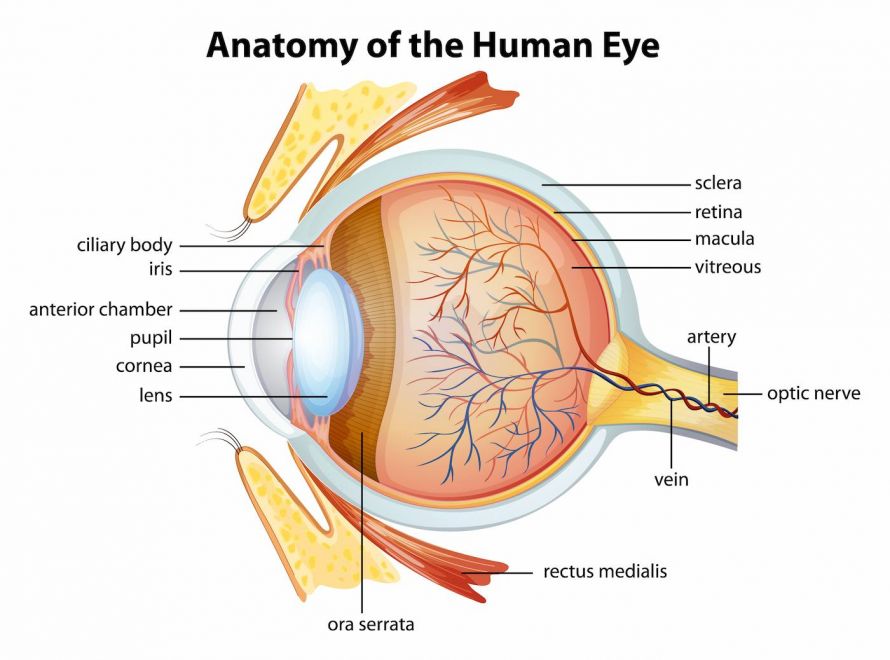
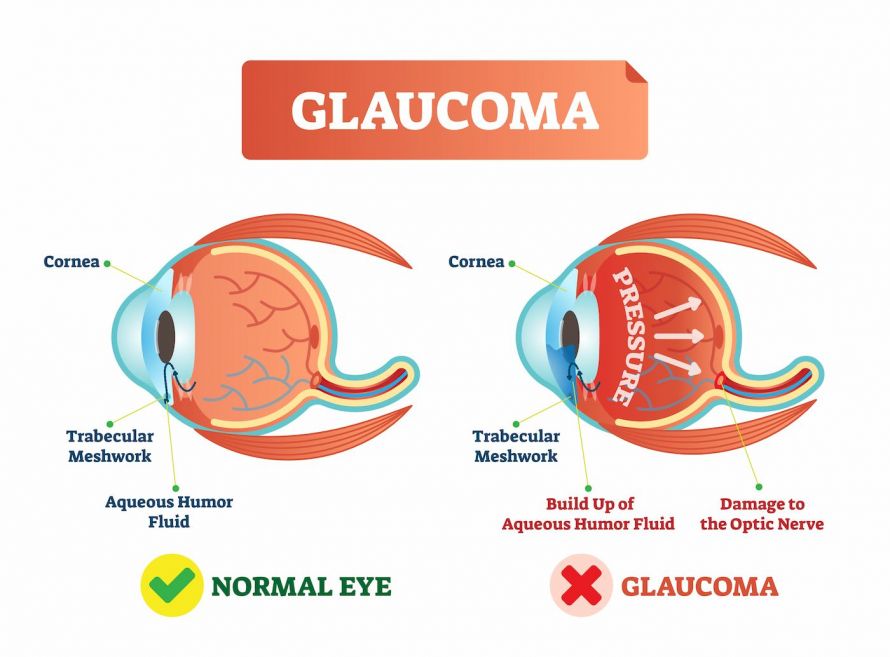
In order to understand the symptoms and development of glaucoma, we will take a look at the Anatomy of the eye:
The eye is spherical and consists of the white outer layer of the eyeball called the sclera. The cornea is the clear “wind shield” of the eye and is located in the front center. Light falls through the cornea onto the iris which regulates the incoming light by narrowing or expanding the pupil.
The lens of the eye lies behind the pupil and is supported by the ciliary muscle. It focuses light and creates a sharp image on the retina which is then transmitted to the visual center of the brain with the help of the optic nerve. The point at which the optic nerve emerges from the eye is called the optic disc or optic nerve head.
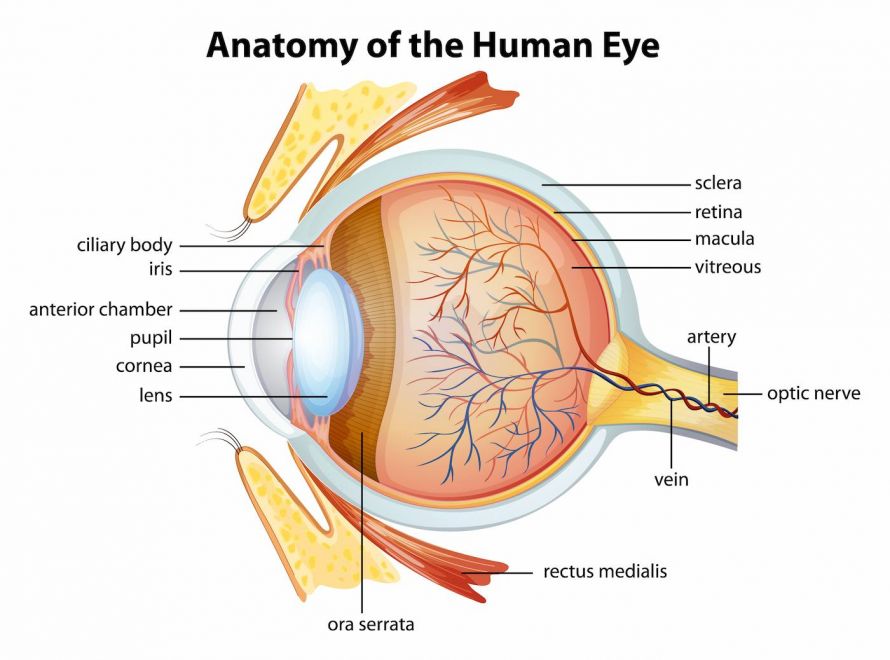
The anterior chamber of the eye is filled with
aqueous humor which nourishes the cornea, iris, and lens. The production of this fluid happens in the ciliary body, and then flows through the pupil into the anterior chamber of the eye. There, it is absorbed into the bloodstream through drainage canals that are located on the outer edge of the iris called the anterior chamber angle or the iridocorneal angle. The production and drainage of this fluid is usually balanced.
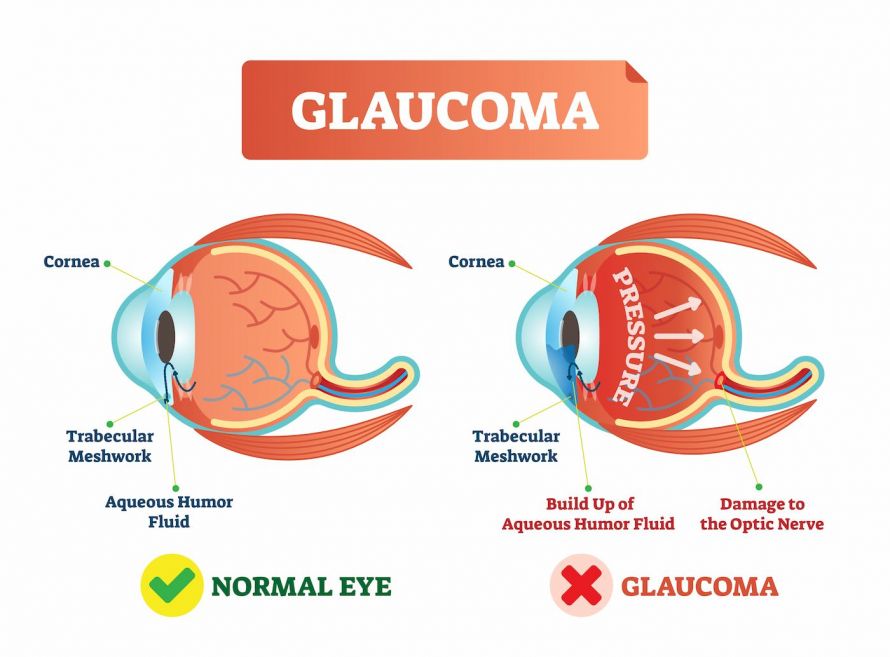
Intraocular pressure is determined by the relationship between aqueous humor production and aqueous humor outflow. This amounts to 10 to 21 mm Hg. The highest values occur at night or in the morning. In older people, intraocular pressure is higher on average than in younger people.
High Intraocular Pressure
If there is an imbalance between intraocular pressure and blood flow to the optic nerve, glaucoma may develop. If the pores of the drainage channels clog, too much fluid will collect in the eye. The pressure within the eye then increases and the blood pressure in the optic disc decreases. This pressure can damage the optic nerve and subsequently impair vision.
Anatomically, a distinction is made between narrow-angle glaucoma and open-angle glaucoma. These terms refer to the posterior surface of the cornea and the anterior surface of the iris, which together are referred to as the anterior chamber angle or iridocorneal angle.
Open-angle glaucoma tends to be more common and is a chronic condition. Narrow-angle glaucoma often leads to a painful glaucoma attack that, if left untreated, can result in blindness.
Any condition that increases intraocular pressure or decreases blood pressure in the optic disc can lead to glaucoma. The optic nerve damage caused by glaucoma can be recognized by the characteristic hollowing of the optic disc. First, it affects the nerve fibers in the middle peripheral retina, and then it progresses to the center.
Risk factors that contribute to the development of glaucoma:
- Very low or fluctuating blood pressure
- encreased pressure in the eye
- genetic predisposition
- blood circulation problems in the hands and feet, tinnitus, or migraines can lead to damage without high intraocular pressure
- Diabetes mellitus
- high myopia or farsightedness
- ethnic groups: People with dark skin are more likely to develop glaucoma than those with light skin
- old age
When approximately 70 percent of the nerve fibers are affected by glaucoma, arcuate visual field restrictions occur in the middle of the visual field. However, this often goes unnoticed by those affected by glaucoma.
Primary Open Angle Glaucoma
Primary open angle glaucoma is the term given to glaucoma that is not caused by any other eye disease.
Primary chronic glaucoma
This type of glaucoma commonly appears around the age of 40 onwards, and it also tends to run in families. With this condition, the drainage area in the anterior chamber angle is blocked due to degenerative changes. Pressure within the eye increases very slowly in this type of glaucoma. Those affected with it do not feel any pain.
A particular type of primary chronic glaucoma is low-tension glaucoma, in which the optic nerve becomes damaged despite apparently normal internal pressure levels. Blood flow to the optic disk is then restricted, because of various factors in this type of glaucoma. This leads to damage to the optic nerve fibers or glaucoma.
Congenital Glaucoma
Occasionally, glaucoma will develop in an embryo. This leads to disruptions in the drainage of the aqueous humor. One common cause of this is a rubella infection during pregnancy. The increased intraocular pressure can lead to the eyeball enlarging.
To prevent permanent deterioration to the child’s eyesight, examinations or possibly an operation must be carried out at an early stage.
If the child has symptoms such as clouding of the cornea, an enlarged corneal diameter, or photophobia, they should be taken to an eye examination as a preventative measure.
Secondary Open-Angle Glaucoma
When open-angle glaucoma is caused by another eye disease, it is referred to as secondary open-angle glaucoma. The diseases that can trigger it include:
- Diabetes mellitus
- intraocular tumors
- an eye injury
- eye inflammation
PEX-Glaucoma
A special type of secondary glaucoma is PEX-glaucoma. With this type, the outflow of aqueous humor is prevented by fine fibrillar deposits in the chamber angle and on the lens. It can cause massive increases in pressure.
Angle-Closure Glaucoma
In narrow-angle glaucoma, the drainage of the aqueous humor is hindered because of a narrow point between the cornea and iris. This results in intraocular pressure increasing steadily, which ultimately leads to damage to the optic nerve or glaucoma.
This type of glaucoma primarily affects people with pronounced farsightedness or advanced cataracts. Intraocular pressure can also increase because of pupil-expanding drugs or anticholinergic agents and lead to a glaucoma attack.
Glaucoma Attack
The iris can suddenly block the anterior chamber angle so that the aqueous humor’s drainage becomes blocked. This leads to a great increase in pressure which makes the eyeball very hard.
Symptoms range from painful and reddened eyes to nausea and vomiting. Sudden vision loss can also often happen.
This is accompanied by very severe headaches, cardiac arrhythmias or seeing colored rings. The pupil sometimes barely reacts or does not react at all to incoming light. A glaucoma attack like this is an absolute emergency.
Normally when diagnosing glaucoma, intraocular pressure is determined using an applanation tonometer. This tool measures the force required to flatten the cornea. Another way of diagnosing glaucoma is taking a measurement with the help of pneumotonometry.
However, measuring intraocular pressure is insufficient to make a glaucoma diagnosis. The following additional tests can also be used to find evidence of glaucoma:
- Perimetry or visual field examination: concerning glaucoma, any arcuate defects are examined here. The patient sits in front of a perimeter, and one of their eyes is covered while the other is supposed to focus on a point in the middle of the apparatus. Points of light then appear in a wide variety of places. If the patient perceives a point, he or she must press a switch.
- Ophthalmoscopy of the optic disc: This determines the shape and size of the optic disc cavity
- GDX (Scanning-Laser-Polarimetry)
- OCT (Optical coherence tomography)
- RTA (Retinal Thickness Analyzer)
- Glaucoma examination with a slit lamp: This can be used to find pigment or protein deposits.
- Examinations for corneal opacities or pigment defects in iris
- Gonioscopy: this assesses the width and potential anomalies of the anterior chamber angle in glaucoma
If the optic nerve is damaged by glaucoma, the intraocular pressure must be permanently lowered. Symptoms like pressure in the affected eye appear differently. The pressure varies and has to be identified through regular checkups. This allows for a subsequent treatment of the glaucoma.
The aim of treatment is to prevent the disease from progressing, because damage that has already occurred cannot be reversed.
The first step in the treatment of glaucoma is medication with eye drops. Surgical procedures can also follow, in which case trabeculectomy is mainly used. Laser trabeculoplasty is an alternative to drug therapy for glaucoma.

Medicinal Therapy
There are numerous options available to treat glaucoma with medications. These include the following drugs which are mainly given in the form of eyedrops:
- Timolol, Levobunolol, Beta-Blocker
- Carbachol, Pilocarpin, Cholinergika
- Brimonidine, Clonidin
- Dorzolamide, Brinzolamide
- Travoprost, Bimatoprost, Latanoprost, Tafluprost
- Cannabidiol
- Cannabinol
The drugs listed above are used to reduce symptoms of glaucoma such as aqueous humor production. Prostaglandins open up a new drainage pathway (uveoscleral drainage pathway). It is possible to combine glaucoma treatment methods. Lifelong treatment is frequently required.
Laser Operation
The following options are available for treatment:
- Cyclodestructive laser: obliteration of the ciliary body
- Cyclocryotherapy: reduction of the aqueous humor produced by the ciliary body through cold therapy
- Argon laser trabeculoplasty: improvement of the drainage at the anterior chamber angle by means of a laser
- Selective Laser-Trabeculoplasty: improvement of aqueous humor drainage
- Neodymium-YAG-Laser iridotomy: Improvement of aqueous humor passage through the creation of an opening in the iris
The results of laser treatment take about six weeks to set in. The intraocular pressure of the patient can be lowered by about 5-10 mm Hg.
Various laser procedures can be used to treat glaucoma
Surgical Interventions
If laser treatment or medications do not stabilize a patient’s glaucoma, an operation can create an artificial drain. The goal of this procedure is to permanently fix the disturbed equilibrium between the fluid production and its drainage. The following procedures are available for this purpose:
- Trabeculectomy und Goniotrepanation: the creation of a drainage fistula on the sclera (dermis)
- Goniotomy and Trabeculotomy: the opening of the trabecular meshwork and connection of the anterior chamber with the Schlemm’s canal
- Iridectomy: pressure equalization through an opening in the iris
- Canaloplasty: insertion of a ring-shaped implant through the Schlemm’s canal
The Patient’s Contribution towards Successful Treatment
It is very important to take the prescribed medications regularly and correctly during glaucoma treatment.
If the doctor prescribes eye drops for glaucoma, it may help to support the hand holding the vial while administering the drops. This is a better way to reach the conjunctival sac of the eye. After the eyedrops have been applied, it is recommended to close your eyes and compress the tear duct for about two minutes. Doing so allows for better drug absorption and reduces any side effects.
When using more than one prescription, you should wait about 15 minutes between dripping the various medications into the eye.
In addition, glaucoma patients should also avoid nicotine. Cigarettes and cigars make the blood flow to the optic nerve even worse. Symptoms should be identified early and reported to your doctor for further treatment.
Basically, you must assume that untreated glaucoma leads to blindness. If damage has already been done because of glaucoma, it cannot be reversed despite therapy.
Primary open-angle glaucoma is a chronic process that is relatively slow. Treatment can stop it from progressing. With a timely diagnosis, adequate treatment can give a good prognosis and alleviate symptoms.
In the case of congenital glaucoma, damage causing reduced visual acuity usually remains. However, total blindness can often be prevented.
To prevent glaucoma, you should have regular checkups with an ophthalmologist. The goal is to recognize glaucoma at its early stage to prevent it from progressing.
Regarding open-angle glaucoma, it is advised to have preventative check ups at least every three years after the age of 40. Symptoms should be carefully monitored and reported to your eye doctor early on.
Patients who have already suffered from an eye injury should have the internal pressure of their eyes checked at least every year.