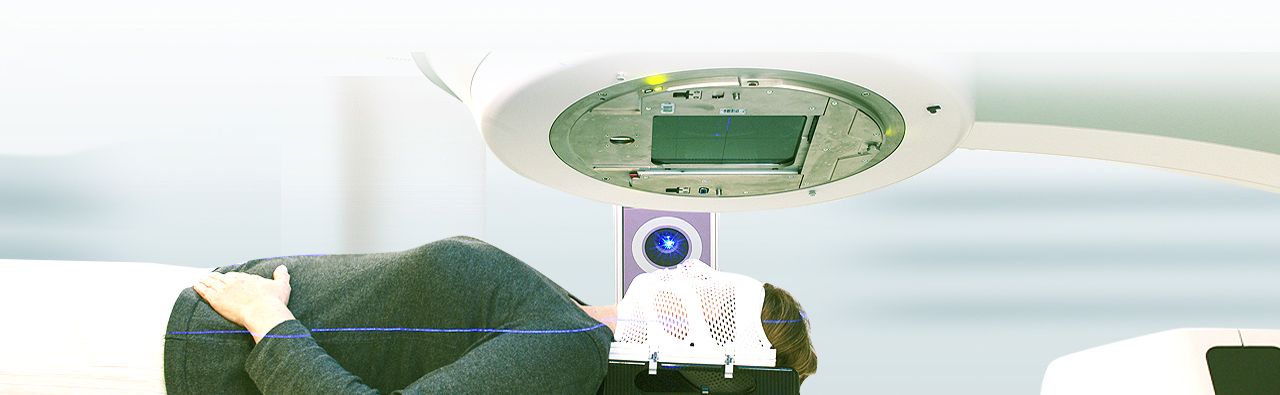
If electromagnetic radiation is able to remove electrons from atoms or molecules, i.e. if it can destroy cells - then radiotherapy is used. This is also referred to as radiation therapy or irradiation.
Positive, i.e. ionising radiation of particles is the foundation of medical radiotherapy. The good thing about it sounds like a contradiction: the radiation has a harmful effect on living cells, i.e. on tissue. It is high-dose radiation that damages the genetic material, both of healthy and diseased cells, i.e. cancer cells. However: the healthy cells survive the procedure and can repair the damage, but the cancer cells die.
Radiotherapy is divided into soft radiation (up to 100 kV), hard radiation (more than 100 kV) and megavolt therapy (more than 1000 kV). Soft radiation is used mainly for superficial tumors, while megavolt therapy is used for deep-seated tumors. In most cases, irradiation is used curatively - i.e. for healing. If it is only a matter of improving the quality of life or alleviating pain, irradiation is also used - in the case of incurable diseases, it is palliative. Irradiation is used alone or in combination with chemotherapy.
Which kind of radiation therapy is chosen depends on many factors, which is why the treatment regime is usually prepared jointly by experts from different disciplines. The most common tumors that are irradiated are breast cancer, lung cancer and prostate cancer.