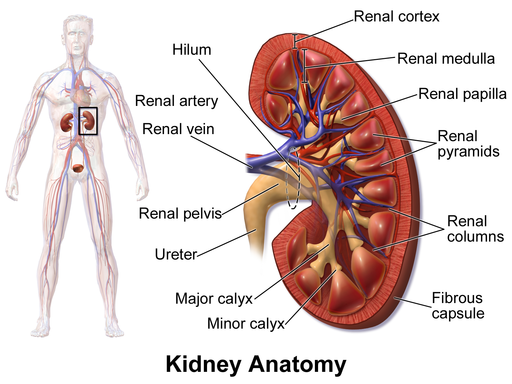
Acute renal failure occurs when your kidneys are suddenly unable to perform their primary function of removing excess salts, fluids and other waste materials from your bloodstream. Once this core ability is impaired and your kidneys lose their filtering ability, your body fluids can soon rise to dangerous levels. In addition, this condition also allows electrolytes and metabolic waste material to build up inside your body, which can also be a life-threatening problem.
Recommended specialists
Article overview
Overview of renal failure
Acute renal failure, also termed acute kidney failure or acute kidney injury, is quite common in people who have already been admitted to hospital. The onset may occur rapidly over the course of just a few hours, or it may take days or even weeks to develop. Those who are critically ill and require intensive care are at the greatest risk of developing acute renal failure.
Though acute renal failure can be a life-threatening condition that needs intensive treatment, it can also be reversible. For anyone who otherwise enjoys good health, there is a chance of recovery.
Symptoms of renal failure
The symptoms of acute kidney failure can include the following:
- bloody stools
- breath odour
- slow, sluggish actions
- generalised swelling in legs, ankles and feet due to fluid retention
- fatigue and tiredness
- pain between ribs and hips
- hand tremors
- tendency to bruise easily
- changes in mood or mental state, especially in an older person
- loss of appetite
- decreased sensation, especially in the hands or feet
- prolonged bleeding
- seizures
- nausea
- vomiting
- high blood pressure
- a metallic taste in the mouth
Causes of renal failure
Acute renal failure can happen for quite a number of reasons. Some of the most common causes are:
- acute tubular necrosis (ATN – a type of kidney injury)
- sudden or severe dehydration
- toxic kidney injury as a result of poisons or specific medications
- auto-immune kidney diseases (e.g. interstitial nephritis and acute nephritic syndrome)
- obstruction of the urinary tract
Any reduction in blood flow can potentially cause damage to your kidneys. The following conditions all pose a risk of a decreased blood flow to the kidneys:
- burns
- dehydration
- haemorrhage
- injury
- low blood pressure
- septic shock
- major illness
- surgical interventions
Some specific disorders can cause blood clots to form within your kidney’s blood vessels, creating a risk of acute renal failure. This includes conditions such as:
- hemolytic uremic syndrome (a disease involving anaemia, acute renal failure and a low platelet count)
- idiopathic thrombocytopenic thrombotic purpura (ITTP – a bleeding disorder)
- malignant hypertension
- transfusion reaction
- scleroderma (tissue hardening)
Certain infections, such as septicaemia and acute pyelonephritis (a bacterial kidney infection), can cause direct harm to your kidneys. Complications during pregnancy, such as placental abruption and placenta previa, can also cause harm to your kidneys.
Diagnosis of renal failure
Acute renal failure is often characterised by generalised swelling, which is caused by fluid retention. During a physical examination, your doctor will check your lungs using a stethoscope to capture any crackling sounds, which usually indicate fluid retention.
Any diagnosis will be supported by some of these tests and procedures:
- urine output will be checked daily
- urine tests will be used to trace any abnormalities suggesting renal failure
- blood samples will be analysed to check levels of urea and creatinine
- ultrasound and CT (computerised tomography) may be used to create detailed kidney images
- a biopsy may be required to obtain a small sample of kidney tissue for laboratory tests
Treatment of renal failure
The aim of any treatment is to restore normal kidney function, though the methods used will vary according to the cause of your acute renal failure. During recovery, it is essential to prevent any build-up of fluid and waste material.
Your diet will be carefully controlled to avoid any accumulation of toxins that your kidneys would normally process. Any recommended diet is likely to be high in carbohydrates but low in protein, salt and potassium.
You may also be given antibiotics to prevent infections, and diuretics to help your kidneys deal with fluids. Calcium and insulin may also be used to stabilise the potassium levels in your blood.
Though dialysis may be required, this is not always the case. During dialysis, an artificial kidney takes over the process of filtering waste from your blood. When blood potassium reaches dangerous levels, dialysis can be a lifesaver.
Chances of recovery from renal failure
Acute renal failure can be a life-threatening illness, and the risk of death may increase where there is:
- a lung disease
- a person of advanced age
- a recent stroke
- blood loss
- evidence of progressive kidney failure
You have a good chance of recovery with proper care and treatment. Always seek immediate medical care for acute renal failure.
Prevention of renal failure
Acute renal failure can be hard to anticipate or prevent. However, taking good care of your kidneys includes:
- following all instructions when taking over-the-counter medications
- following your doctor's advice on managing any health condition
- adopting or maintaining a healthy lifestyle, which includes a balanced diet and regular exercise