The discipline of addresses the interactions between the hormonal and nervous systems. The human body uses hormones as important messengers, not only for communication between the central nervous system and other areas. They also have an important role to play within the brain. However, if the sensitive system gets out of balance, the consequences are often far-reaching. Numerous unspecific symptoms can emerge, which necessitate examination by an experienced neuroendocrinologist, who measures the hormone level and considers the complex interconnections between hormones and the nervous system.
Article overview
Neuroendocrinology - Further information
The complex interplay between hormones and the nervous system
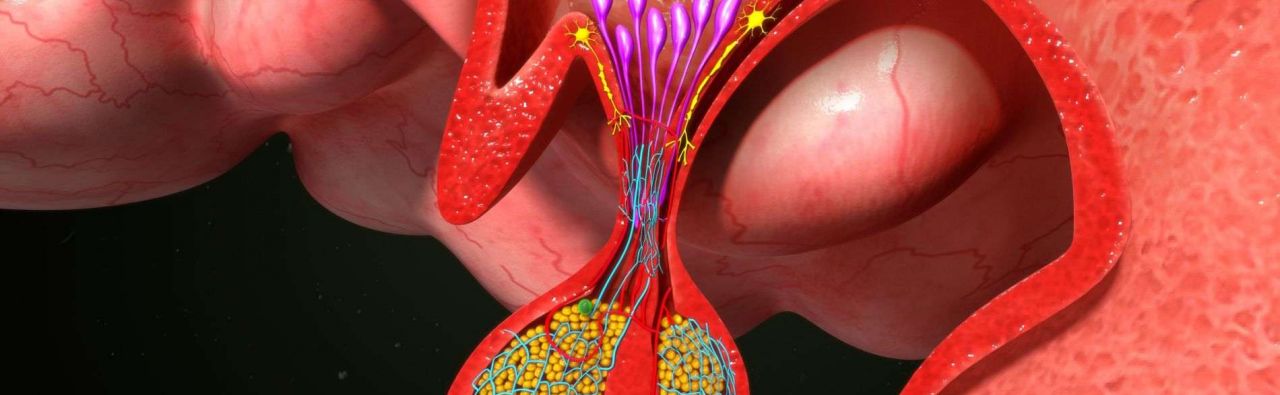
The two most vital structures in neuroendocrinology are the hypothalamus and the hypophysis (pituitary gland). Both are located in the brain, from where they control functions essential for survival. Amongst other things, the hypothalamus is responsible for hunger, thirst, a healthy day and night rhythm, body temperature and an even blood pressure. All these issues are regulated by the increased or reduced production of the appropriate controlling hormones.
The hypothalamus itself produces no hormones, which are distributed via the blood circulatory system throughout the body. Instead of that, it only addresses the hypophysis, also known as the pituitary gland, where many of the controlling substances are produced. In turn, the messengers dispatched by the hypothalamus control the production of hormones by the pituitary gland, which then control a very wide variety of body functions ranging from the thyroid gland through the adrenal glands to milk production in the female breast.
Diagnostics in neuroendocrinology
If the hormones in the human body become unbalanced, the first step is to identify the precise location of the malfunction. This is achieved generally by establishing the hormone level. If the thyroid gland is underactive, but the thyroid gland itself is healthy, then the cause of the disorder is very probably in the brain.
In most cases, neuroendocrinologists have also had specialist medical training as an endocrinologist, but sometimes they are also internists or neurologists who have specialized in this field. Quite a few of them have also trained in several specialist medical fields, which gives them a better understanding of the complex regulatory circuits involved in the pituitary gland-hypothalamus system.
Apart from the hormone levels and endocrinological functional diagnostics mentioned above, other important diagnostic techniques are imaging procedures. Pathological changes in the brain area can be made visible through CT, MRT or ultrasound. Knowing exactly which structures are affected helps the neuroendocrinologist select the right treatment method. If a particular malfunction is specifically suspected, the doctor will give the patient certain substances at frequent intervals and then check by reference to the response how particular regulatory circuits are functioning.
The specialist field of neuroendocrinologists: functional disorders of the pituitary gland
The causes of neuroendocrinological malfunctions are many and varied. Doctors generally distinguish here between hypofunction and hyperfunction. In hypofunction (or underactivity), too few or no hormones are produced so that all the regulatory circuits controlled by this hormone are affected. In hyperfunction (or overactivity), there is a pathologically increased level of production, mostly because of structural changes in tissue. All malfunctions can affect only one particular, several or all hormones which are produced in the pituitary gland.
In some circumstances, neuroendocrine hypofunction occurs because of a defective gene, which means that the problem is congenital. Treatment consists in administering the missing hormones to prevent the impairments that would otherwise occur. Depending on which gene defect is present, treatment can be temporary or lifelong. The same applies if brain tissue has been destroyed by an accident or operation and so no longer produces sufficient hormones.
The cause of neuroendocrine hyperfunction is generally a tumor in the pituitary gland. In most cases, these are benign swellings where the treatment depends mainly on their size and growth. If the tumor increases in size quickly, the best solution is generally an operation. This also applies to hypophysitis, i.e. inflammation of the pituitary gland. However, in some cases medication-based treatment is sufficient.
No less importantly, neuroendocrinologists are important points of contact in transsexual gender changes. They regulate and control the hormone therapy and ensure that the switch in gender hormones proceeds as subtly as possible for the body without incidents.
Neuroendocrinologists – experts in the hormone balance in the brain
Neuroendocrinologists must not only be experts in matters concerning the pituitary gland and its many regulatory circuits. They must also listen to their patients precisely and attribute the symptoms they describe to possible causes. By means of specific hormone diagnostics and imaging techniques, they discover where the faults in the system are and launch suitable treatment.