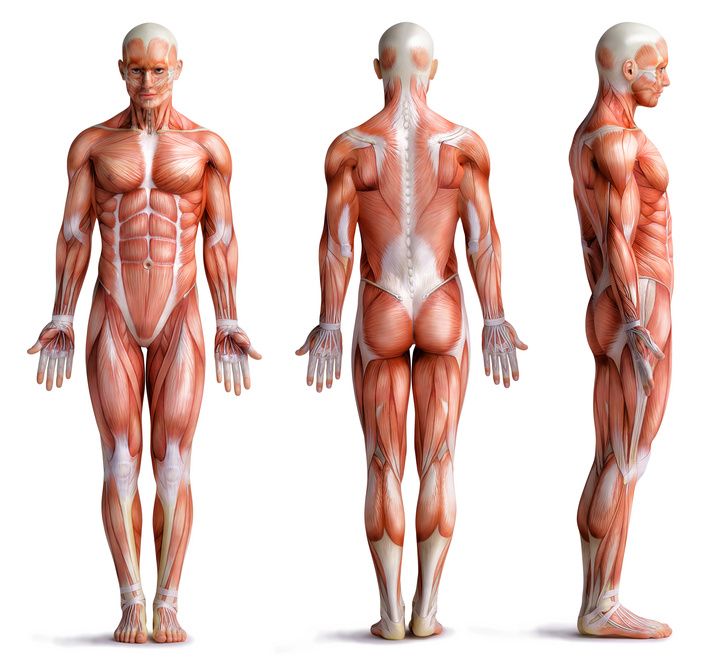
Over 600 muscles support and move the body. They are also involved in various organ functions.
Muscular dystrophy: (ICD code: M62.5) basically means the loss of muscle mass. There are various causes for this, including
- Being bedridden,
- Injuries to the nervous system,
- Metabolic diseases as well as
- over 700 possible genetic disorders.
Muscle dystrophy can also be congenital.
The disease affects relatively few people. In Germany, an estimated 50,000 to 300,000 people live with muscular dystrophy.
Muscular apparatus of the human being © adimas / Fotolia
Muscle diseases and muscular dystrophy have not yet been fully scientifically researched.
Around 800 forms of muscle diseases are now known. For this reason, it has not yet been possible to provide medicines that are tailored to the different forms of muscle dystrophy.
Depending on the severity and context of the disease, the course of muscle dystrophy can vary greatly. Some people are barely restricted with this condition. Others can develop severe symptoms in a relatively short period of time. Premature death is also possible.
Muscular diseases progress spasmodically, i.e. irregularly and with varying degrees of progression.
In the majority of cases, a cure is not possible, even spontaneous healing by natural means does not occur.
Muscular dystrophy owing to lack of exercise
If muscles are not used, the body breaks them down because muscles need a lot of energy. With physical inactivity and confinement to bed, many muscles therefore regress. Seniors with an inactive lifestyle are especially at risk of this type of muscle loss.
After a few days of bed rest, this phenomenon is already clearly noticeable. Patients then complain of lack of energy and feeling listless. They then need some time to regain strength and their former activity level.
That is why patients are mobilised as quickly as possible with physiotherapy during a hospital stay. Then the musculature remains largely intact.

Mobilisation and exercise prevent muscular dystrophy in old age. © gewitterkind / Fotolia
Muscular dystrophy as a disease in its own right
Muscle dystrophy as a neuromuscular disease, on the other hand, affects nerves and muscles. The disease progresses unceasingly.
If the muscles themselves are diseased, we speak of myogenic muscle atrophy, also known as myodystrophy or myopathy.
We speak of neurogenic muscle dystrophy when the cause lies in the cells that supply the nerves.
The myogenic forms include
- Duchenne muscular dystrophy type (DMD) and
- Becker muscular dystrophy type (BMD).
These diseases occur almost exclusively in the male sex.
In Duchenne muscular dystrophy, there is a defect in the gene for dystrophin. Dystrophin is found in the cell membrane of muscle fibres and plays an essential role in muscle contraction. If this protein is missing, as is the case in children with DMD, motor development disorders occur.
Most children with DMD can never jump or run and their gait is unsteady. Between the ages of 6 and 13, they usually lose the ability to walk independently. Due to heart muscle disease or inadequate breathing, patients usually die in early adulthood.
In contrast, Becker muscular dystrophy results in a deficiency of dystrophin due to gene mutations. This also results in progressive muscle dystrophy and weakness. However, life expectancy is only slightly limited or not limited at all.
Known forms of neurogenic muscular dystrophy are
- Werdnig-Hoffman disease (proximal spinal muscular atrophy type 1, SMA1) and
- Kugelberg-Welander disease (proximal spinal muscular atrophy type 3, SMA3)
The diseases were named after the scientists who researched them. The diseases are also genetically inherited, but occur in boys and girls.
SMA3 only manifests itself after learning to walk, through difficulties in walking etc. It progresses only slowly.
SMA1 occurs within the first three months of life. It is much more pronounced in terms of symptoms.
Children with SMA1 often die within the first 2 years of life; in children with SMA3, life expectancy is usually normal.
Amyotrophic lateral sclerosis (ALS) is a neurodegenerative disease. It only appears in older adulthood. The mean age of onset is about 60 years.
In ALS, damage occurs to certain nerve cells (motor neurons) in the central or peripheral nervous system. This influences the musculature and thus the motor function. Depending on which motor neurones are affected, the following may occur, among other things
- Walking disorders,
- Twitching,
- Paralysis,
- Discomfort on the skin,
- Speech disorders and
- Swallowing difficulties
may occur. The paralysis continues to progress. Therefore, the disease usually leads to death within a few years due to respiratory failure.
Only about 5 to 10 percent of ALS cases are familial (inherited); most develop spontaneously.
The most important causes of muscle atrophy at a glance:
- Age or malnutrition
- Physical inactivity or (necessary) bed rest
- Genetic mutations, causing disturbances in muscle activity and the nervous system
- Autoimmune diseases
- Other diseases such as cancer or HIV infections
The first signs of muscular dystrophy are often overlooked or downplayed. They can be
- difficulties with everyday movements, for example climbing stairs and walking, or
- swallowing and speech disorders.
sein. Altered posture is also one of the symptoms. The skeletal muscles are then no longer able to fully support the skeleton.
Children with congenital muscle weakness due to a genetic defect show slower physical development. Compared to children in their age group, their movement patterns are atypical, for example, when
- sitting down,
- standing up or
- walking.
Paediatricians therefore monitor the child's developmental progress during regular examinations.

Physiotherapy helps children with muscular dystrophy © Picture-Factory / Fotolia
An early diagnosis already at birth helps affected children. Suitable treatments and orthopaedic aids promote the child's physical development.
Affected people with muscle dystrophy feel a distinct lack of strength. They may also suffer from impaired organ function.
The musculature continues to waste away,
- it is difficult to breathe,
- the digestive activity is restricted and
- the heart is weakened.
If the disease is severe, the muscle dystrophy brings vital organ functions to a standstill. If the breathing or the heart is affected, muscular dystrophy becomes a life-threatening disease.
Muscular diseases also develop in multiple sclerosis. However, muscular dystrophy is only partly related to multiple sclerosis. The difference lies mainly in the causes and symptoms.
Multiple sclerosis is a chronic inflammatory disease of the nerves. The myelin sheath, i.e. the electrically insulating outer layer of the nerve fibres, is destroyed in stages. Multiple sclerosis is therefore a neurological disease in which muscle cell disorders occur as a result.
Multiple sclerosis is also known as the "disease of 1000 faces" because the symptoms can be extremely varied: Muscular dystrophy is one of them.
Muscular dystrophy affects the whole body and its functions. Therefore, patients with muscle wasting need comprehensive therapeutic care for all areas of life. A cure is only available for muscle wasting due to inactivity. Otherwise, only the discomfort can be alleviated.
The aim of the treatment is to improve the quality of life and life expectancy. The independence of the person concerned should also be increased. The following treatments and methods are used:
- Physiotherapy with special exercises for strengthening and mobility
- Occupational therapy for the training of activities of daily living (ATL/ADL)
- Electrotherapy
- Massages and baths
- Ultrasound therapy
- Speech therapy (speech training) and swallowing therapy
- Support measures for respiratory and cardiac functions, such as respiratory support
- Early treatment of infections and complications
- Operations such as tendon shortening or surgery on the spine
- Provision of aids for walking and standing (e.g. a rollator) or a wheelchair
- Psychological care and socio-medical support also for relatives
- Drug treatment of the underlying disease (for example, steroids for Duchenne muscular dystrophy or riluzole in ALS)
Enzyme replacement therapy helps some sufferers, such as those with Pompe's disease, a glycogen storage disorder. Enzyme replacement therapy is a treatment with special proteins that are missing in the body of some patients. Enzyme replacement therapy is a procedure that is similar in principle to diabetes treatment. It usually replaces the missing metabolic building block on a lifelong basis.
There have also been initial successes in the field of gene therapy in the laboratory. For example, in spinal muscular atrophy, the defective genes can be replaced by functional genes. The body can then produce the missing proteins again.
Doctors have high hopes that rare, hereditary neuromuscular diseases can be treated with gene therapy methods in the future.
The prognosis depends on the causes of the muscular dystrophy. However, if the disease is based on a genetic disorder, muscular dystrophy is considered irreversible and incurable.
The respective form of the muscle or neurological disease determines the progression and life expectancy of those affected. There are cases with such a slow progression that life expectancy and quality of life are hardly limited. In unfavourable progressions, the muscle function decreases rapidly. Affected people usually die in young adulthood, sometimes even in infancy.
However, the reduction of muscle mass can also be a consequence of inactivity. Therefore, mobilisation and mobility are important support measures for seniors and bedridden persons.