A sunken chest(pectus excavatum) is a malformation of the chest. It manifests as a funnel-shaped depression of the chest area towards the back in the direction of the spine. The sternum and the cartilage connections between the sternum and the ribs (rib cartilage) are affected.
Sunken chest is the most common malformation of the human chest. It occurs with a frequency of about 0.1 to 2 percent. Boys are about 3 times more likely to be affected by this thoracic deformity than girls.

Sunken chest in a man © jupiter8 | AdobeStock
The cause of this malformation has not yet been conclusively clarified. However, there are indications that
- it is caused by a weakness of the anterior chest wall or
- mechanical factors play a role in the development.
In up to 40 percent of cases, there is a familial predisposition. It is therefore assumed that genetic reasons are also partly responsible for the development of sunken chest.
In addition, the sunken chest occurs more frequently in various syndromes, for example
- Marfan syndrome,
- Poland syndrome and
- Foetal alcohol syndrome.
A sunken chest can usually be seen directly after birth. In the course of further body growth, the malformation increases. Since the rib cage is still flexible, the heart and lungs adapt to the anatomical situation in the thorax. That is why children and adolescents often have no physical symptoms.
However, with increasing age and age-related sinking, physical discomfort may occur. In this way, the misalignment of the ribs can be transferred to the spine and lead to poor posture.
The shoulders are then often tilted forward, the abdomen protrudes and the spine is curved backwards (kyphosis). As a result, the intervertebral discs are exposed to greater stress, which leads to back pain.
If, due to the incorrect posture, there is increased pressure on the stomach, heartburn can occur. Occasionally, sunken chest also causes symptoms such as
- Shortness of breath,
- Palpitations and
- Quick fatigability
finger. In most cases, however, the lung function and heart examinations rarely show any pathological findings.
As children and adolescents often suffer from the deformity, psychological abnormalities can develop. For example, some reject their bodies, do not exercise and withdraw from their social environment.
If there are no symptoms, there is therefore rarely an indication for a sunken chest operation for medical reasons.
Sunken chest surgery may be necessary if the heart or lungs are severely displaced and physical symptoms occur.
General measures for the treatment of a sunken chest
As a general rule, treatment in childhood tends to be cautious. Sunken chest surgery is rarely indicated. Instead, the progression of the development of the sunken chest is checked regularly.
Physiotherapy and posture training are also recommended. Adolescents and adults can prevent incorrect strain on the intervertebral discs by exercising their back muscles. Muscle and fitness training can also be useful.
Sunken chest correction with suction cup
Instead of sunken chest surgery, suction cup treatment can also be considered.
In the process, a suction cup specially adapted to the patient's anatomical conditions slowly pulls the chest upwards. Usually, the first application of the suction cup is done on an outpatient basis in a hospital so that the doctor can check that it is being used correctly.
The duration of treatment depends on the severity of the condition and also the general health of the patient. If necessary, the suction cup must be used up to several times a day for up to several hours over two to three years. Long-term results are still pending, but the first results are promising.
Sunken chest surgery is necessary for
- Restrictions of physical functions (such as breathing or heart function) or
- Psychological stress due to the sunken chest.
Today, the decision to have a sunken chest operation is mostly made for psychological and/or cosmetic reasons.
In children, sunken chest surgery is only advised in rare cases.
Adolescents and adults often suffer from the psychological-cosmetic stresses. Therefore, they usually express the wish for a sunken chest correction themselves.
The aim of sunken chest surgery is to correct the sunken chest as completely as possible while avoiding large surgical scars. For this reason, minimally invasive procedures are increasingly used today instead of conventional open procedures.
The following are mainly used
- the minimally invasive sunken chest operation according to Nuss (MIRPE) and
- sternochondroplasty (Erlangen sunken chest surgery).
The methods of sunken chest surgery according to Ravitch or Rehbein, which used to be performed more frequently, are increasingly being abandoned. These are very complex and stressful procedures for the patient. From a cosmetic point of view, an unflattering incision is necessary. This is followed by a hospital stay of 14 to 21 days.
Preliminary examinations in preparation for sunken chest surgery
The full extent of the sunken chest can only be visualised using imaging techniques.
By means of pulmonary function test and ECG or Echocardiography, the doctors look for disturbances of the heart function and respiratory impairments.
The examinations are usually carried out at the hospitals that also perform sunken chest surgery. The examination results are then sent to the appropriate specialist clinic in preparation for sunken chest surgery.
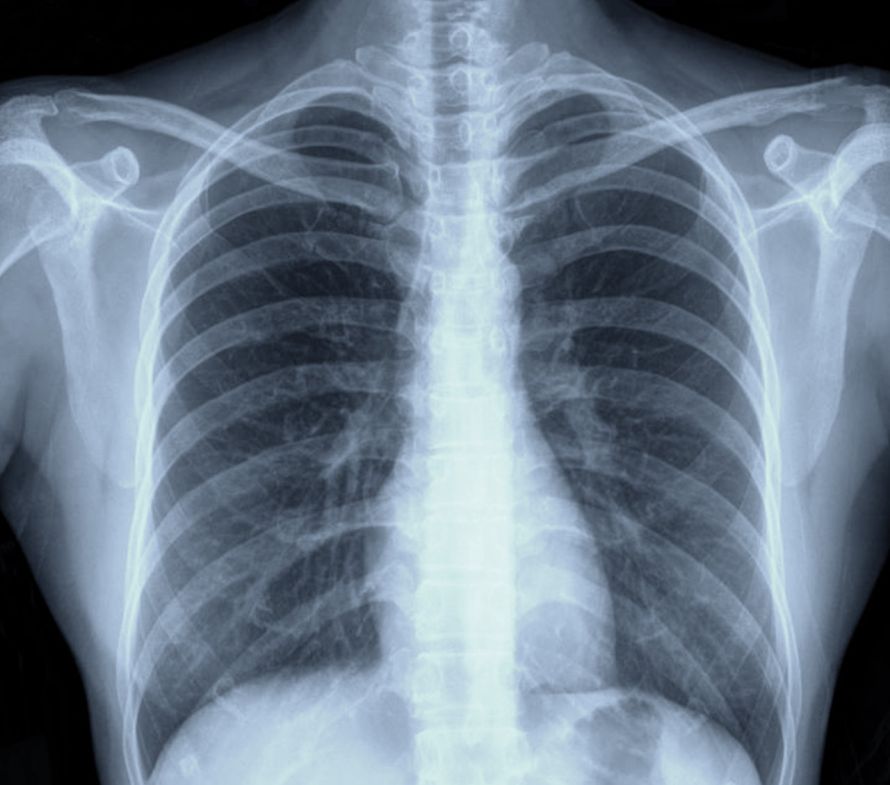
X-ray examination (CT scan)
Important imaging methods are the classic X-ray or better the computer tomography (CT). A CT provides a more detailed picture than the X-ray. Both procedures can show the bones, including the ribs and the sternum.
Bone and other dense tissue absorb X-rays more strongly than less dense tissue (e.g. the skin). In this way, the ribs and the sternum with the kink can be identified and the exact extent of the sunken chest can be determined.
The X-ray examination is used
- in preparation for a sunken chest correction and
- to exclude other diseases (e.g. of the spine).
verwendet.
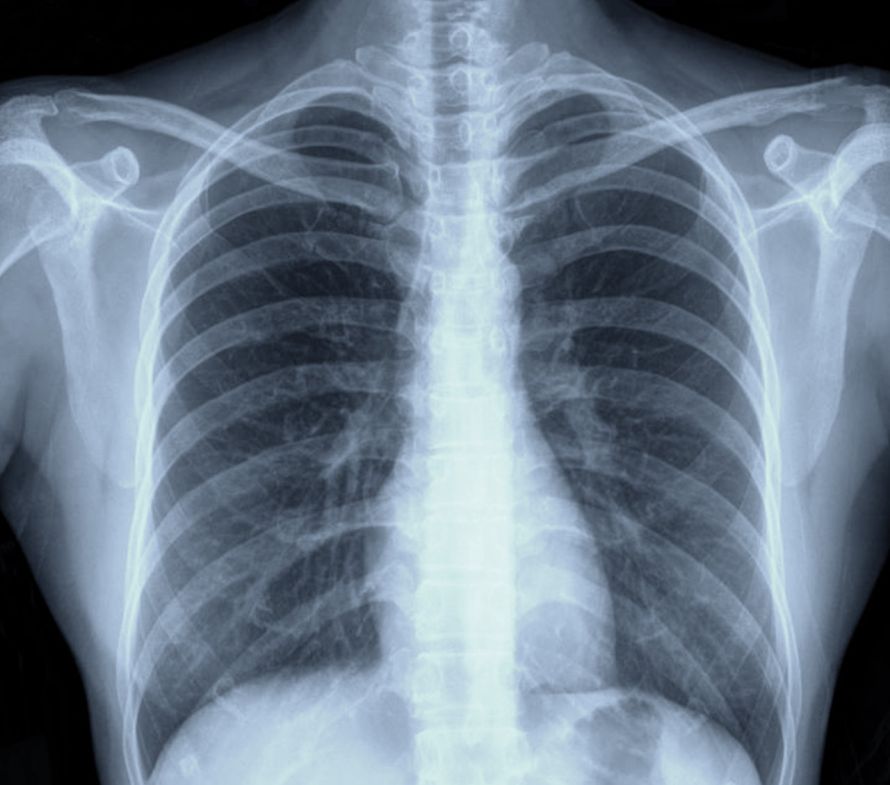
A chest X-ray is an important tool in the evaluation of a sunken chest © jupiter8 | AdobeStock
Magnetic resonance imaging (MRI)
With the help of Magnetic resonance tomography high-resolution sectional images can be displayed in detail. In contrast to CT, it also shows the soft tissue.
MRI can be used to determine the extent of the sunken chest, such as the sunken depth and diameter.
Unlike an X-ray examination, there is no radiation exposure with an MRI.
Haller index
The sunken depth can be used to objectify the extent of a sunken chest. The Haller Index displays the relationship between
- the transverse diameter of the rib cage and
- the distance between the lowest point of the depression and the spine.
ins Verhältnis zueinander.
If the Haller index is 3.2 or higher, a recommendation for sunken chest surgery is often made.
Pulmonary function test
The lung function test provides information about the extent of the restriction of lung function as a result of a sunken chest.
For example,
- the lung volume,
- the expiratory reserve volume (ERV),
- the inspiratory vital capacity (IVC) and
- the forced vital capacity (FVC)
is determined. This allows the extent of any functional limitations to be determined and the need for a sunken chest correction to be assessed.

A pulmonary function test can give an indication of the extent of the sunken chest © mjowra | AdobeStock
Echocardiography
Echocardiography can be used to assess any impairment of the heart valves and certain heart functions.
This can also be used to assess the need for sunken chest correction.
Stress ECG
The sunken chest can also lead to impaired cardiovascular function (e.g. cardiac arrhythmia). Cardiac arrhythmia) may occur. A stress ECG can assess heart function during physical activity.
This can also help to assess the need for sunken chest surgery.
Minimally invasive sunken chest surgery according to Nuss (MIRPE)
In the Nuss sunken chest correction, only two small incisions are made under the armpit on the lateral chest wall. They do not interfere cosmetically later.
Through these incisions, a pre-bent metal bracket is inserted under the sternum at the level of the depression. The metal bracket is adapted to the patient's anatomy in advance. The surgeon checks the correct fit using a video camera (thoracoscopy).
The bracket, which is made of steel or, for allergy sufferers, titanium, is fixed to the side, leaving the sternum itself intact. This pushes the sunken sternum and the affected ribs with the deformed rib cartilages outwards again.
In some cases, two or even three metal brackets are also required.
The sunken chest correction is performed under general anaesthesia and takes about 50 minutes. The two small lateral incisions heal quickly without any disturbing scarring. After the sunken chest operation, the external cosmetic success is immediately visible, the chest has acquired a "normal" shape.
Surgery-related complications are also rare. Therefore, the patient can leave the hospital after only a few days.
Already after about three months, the patient can resume a completely normal life with all the usual activities.
After two to three years, the metal brackets are surgically removed again. In older patients, it may be necessary to leave the metal brackets in the body for longer.
As the chest wall must still be flexible for this type of sunken chest correction, it is particularly suitable for younger patients.
Very good results can be achieved with this sunken chest correction, especially with symmetrically shaped sunken chest The best time for sunken chest surgery according to Nuss is the end of puberty, although later procedures are also possible.
Minimally invasive sunken chest surgery according to Rokitansky
A further development of the sunken chest operation according to Nuss is the minimally invasive sunken chest correction according to Rokitansky.
This is characterised, among other things, by
- notching of the sternum,
- thoracoscopic slits of the rib cartilages and
- through the use of a metal bracket that consists of only one piece.
aus. This prevents metal abrasion in the body.
Open sunken chest surgery: Sternochondroplasty (Erlangen sunken chest correction)
The Erlangen sunken chest operation is also known as the minimalised Erlangen correction method (MEK). It is based on the methods according to Ravitch/Rehbein/Wernicke. In these methods, the chest is opened through an incision several centimetres long, which is vertical in the case of men or horizontal in the case of women.
The deformed ribs are then separated from the sternum and the cartilage on the deformed ribs is removed. After the sternum has been sawn, it is lifted and fixed with metal brackets. The thorax is then closed again.
In the sunken chest operation, which was further developed in Erlangen, the ribs are not completely separated. Instead, they are only notched at the base of the sternum. The sternum is then stabilised in the raised position. This is done by inserting one or two metal brackets through a small incision in the lateral chest wall. The metal brackets can be surgically removed after just one year.
The Erlangen sunken chest correction is a relatively gentle surgical procedure. Similar to the Nuss sunken chest operation, the patient can leave the hospital after just a few days.
It can be used for both symmetrical and asymmetrical deformities and is suitable for all age groups (including older patients).
After several decades in clinical use, the Erlangen sunken chest correction can show very good long-term results.
Every sunken chest operation, like any other surgical procedure, involves certain risks. This can lead to wound healing problems, which can be the result of the mechanical intervention or an infection of the wound.
Very rarely, severe infections and allergic reactions to the metal brackets occur. These must then be removed prematurely. If allergies (e.g. nickel allergy) are known, special temples made of titanium can be used.
Any pain that may occur after the operation can be treated efficiently. As a preventive measure, anaesthetists can place a peridural catheter (PDK) during sunken chest surgery. The activity of the nerves in the thoracic region can be manually controlled via this.
This makes it possible to control the pain treatment after sunken chest correction and thus achieve complete freedom from pain.
Depending on the sunken chest operation used, a hospital stay of about 6 to 11 days, sometimes up to several weeks, may be necessary. Mobilisation usually starts from the first day after the sunken chest operation. However, strong twisting movements of the upper body should be avoided for the first 8 to 12 weeks after sunken chest surgery.
At regular intervals, the corrected sunken chest should be checked by means of X-ray examination. In addition, the muscles should be strengthened under physiotherapeutic guidance. Normal weight-bearing of the upper body is usually possible after three months. If heavy physical exertion is planned, the stability of the sunken chest correction should be checked beforehand.
Depending on the sunken chest operation, the metal bracket or brackets are either
- already after one year (Erlangen sunken chest correction) or
- after about three to four years (sunken chest, sunken chest correction according to Nuss)
removed by means of a final surgical procedure.