Known in German as "chronische Polyarthritis", it is the most common inflammatory disease of the joints.
The most important characteristics of the disease can be found in the German term:
- Chronische or chronic stands for the long duration of the disease,
- Arthritis means inflammation of the joints, and
- Poly indicates a variety of affected joints.
In Germany, rheumatoid arthritis is known as "chronic polyarthritis" or its synonym "polyarthritis", which merely means having arthritis in five or more joints in English.
Rheumatoid arthritis is a chronic inflammatory systemic disease. It starts in the
- Synovial membrane,
- Tendon sheaths, and
- Bursae
and leads to damage of the joints, tendons, and bones. The small joints of the hands and feet are at risk, as are the large joints of the upper and lower extremities. The final stage of the disease can be severe disability.
This video shows the progression of the disease at the hip joint:
Worldwide, about 0.5 to 1% of all people suffer from rheumatoid arthritis. In Germany, it is estimated that approximately 800,000 people suffer from the disease, with women being affected approximately three times more often than men. The disease can occur at any age, most commonly between the ages of thirty and fifty.
The development of rheumatoid arthritis is an immunological process. This leads to uncontrolled immune system activity, resulting in permanent inflammation.
A genetically determined different reactivity of the immune system is probable for rheumatoid arthritis.
Research has made many advances in understanding rheumatoid arthritis in recent years. Nevertheless, the cause of the disease is still not clear.
A malfunction of the immune system is conceivable: In this process, cells of the immune system attack the body's own substances (e.g., articular cartilage). That is why rheumatoid arthritis is classified as an autoimmune disease.
At the onset of illness, infectious agents (viruses or bacteria) could also play a role. To date, this has not been confirmed. A hereditary predisposition is probably also necessary. This predisposition would lead to the outbreak of the disease when coming into contact with certain infectious agents. It also affects the severity of rheumatoid arthritis.
Inflammation-promoting tissue hormones called cytokines also play an important role.
New possibilities for the treatment of rheumatoid arthritis are emerging from the research findings of recent years. They may also offer hope for a better prognosis, even if the cause of the disease is unknown.
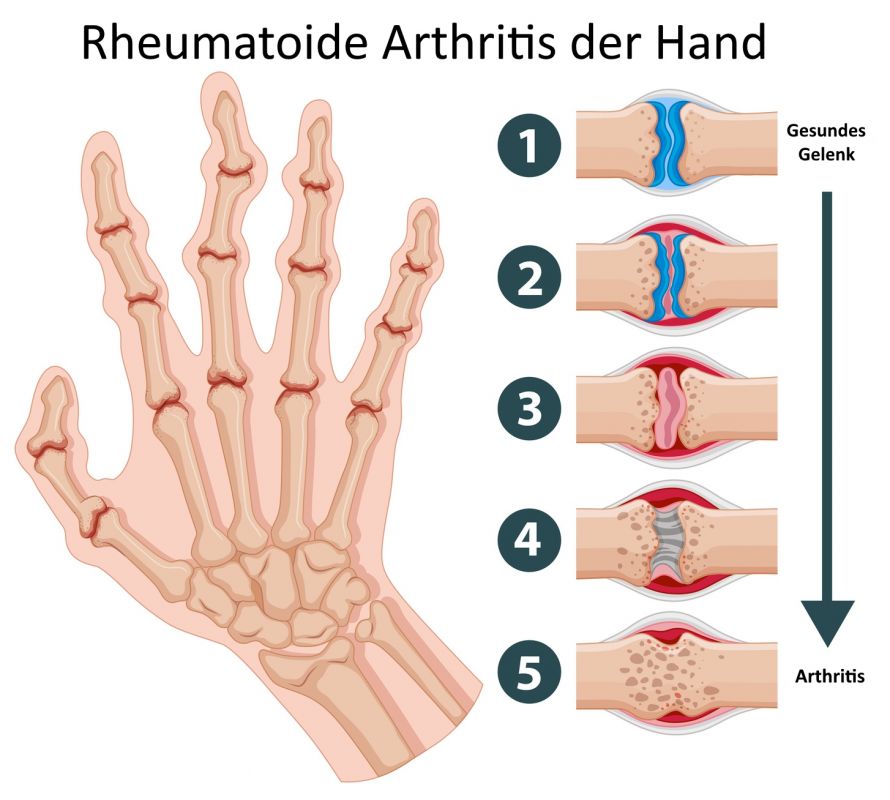
At the center of the disease process is the synovial membrane altered by inflammation (pannus). The inflammatory growths of the synovial membrane overgrow the articular cartilage.
The ongoing inflammation develops messenger substances and enzymes that further damage the cartilage. The pannus can also grow into the bone and attack the cartilage from the edge of the joint.
The pannus and joint effusion are followed by the painful movement disorder with musculature degradation.
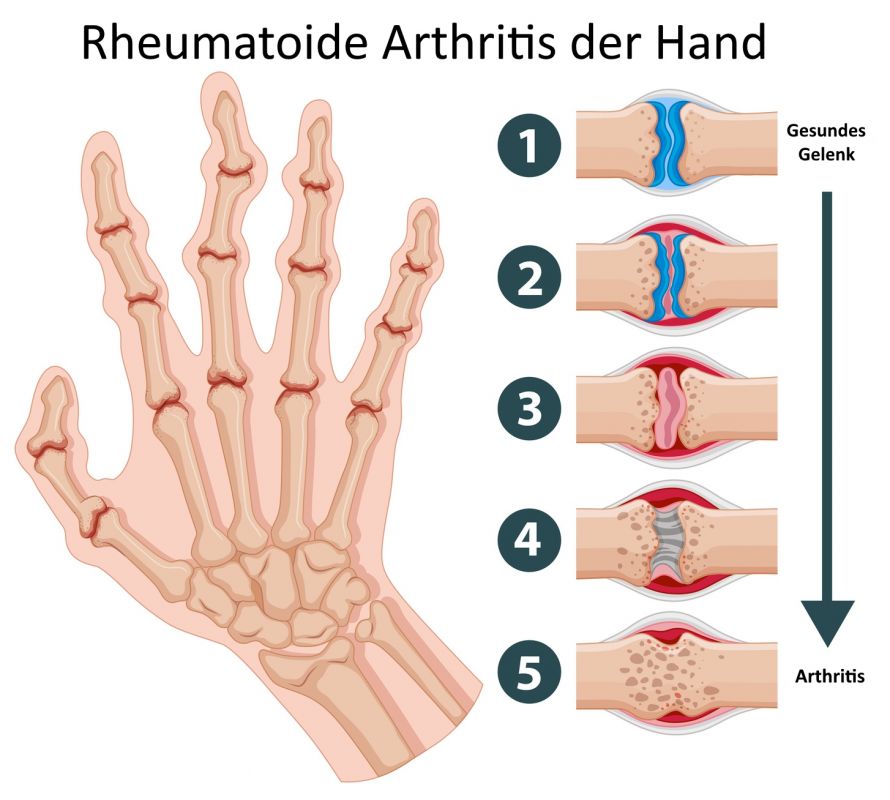
Joint destruction in rheumatoid arthritis © GraphicsRF / Fotolia
In later stages, the joint capsule becomes scarred with increasingly restricted movement. Other courses show a progressive destruction of the cartilage and bone with sometimes serious deformities of the joints (mutilation).
The end result is a contracted, destroyed joint with
- Gross deformation of the joint-forming bone parts,
- Instability, and
- Connective tissue stiffness.
The cartilage damage leads to secondary osteoarthritis. It may overlay the clinical picture and even dominate in late cases.
Pathways of joint destruction in rheumatoid arthritis (according to Mohr):
- Cartilage destruction via the synovial fluid
- Proliferating synovial tissue (red pannus tissue) overgrows the cartilage and destructively invades it
- Proliferating synovial tissue pushes between cartilage and bone
- Proliferating pannus tissue invades the bone marrow
- From the medullary cavity, pannus tissue again spreads to the cartilage
Rheumatoid arthritis develops gradually or progresses in spurts interspersed with periods of apparent inactivity.
The early stage is indicated by
- Symmetrical, spongy joint swellings (especially at the middle and base joints of fingers and toes),
- Morning stiffness,
- Pain.
However, atypical spread with acute affliction of large joints also occurs. Rheumatoid nodules may develop on the extensor surfaces of the extremities.
The stages of progression are extremely varied. They range from occasional spurts of joint symptoms to progressive joint destruction.
Affliction of the synovial upper cervical joints is a special feature. It can lead to displacement of the head relative to the cervical spine and cause damage to the spinal cord. This results in varying degrees of sensory and motor dysfunction.
In late stages, the characteristic deformities persist. These include
- Ulnar deviation of the long fingers,
- A prominent ulna head,
- Swan-neck deformity and boutonnière deformity of the long fingers, and
- Loss of function due to tendon rupture.
Pain and limited mobility are most pronounced in the morning. The immobility on waking is called morning stiffness. Depending on the disease activity, this morning stiffness can last for several hours.
In addition to this typical onset of rheumatoid arthritis, occasionally only a few large joints are inflamed at the beginning. In old age, they’re often the shoulder joints.
Over the course of weeks or months, more and more joints may become diseased. Besides the joints, the tendon sheaths become inflamed and swell (e.g., the finger extensor tendons on the back of the hand). The spine (usually the cervical spine) and bursa can also be affected, the latter often at the elbow.
General symptoms, such as
- Fatigue,
- Listlessness,
- Fever,
- Night sweats, and
- Possible weight loss,
indicate that the whole body is affected by the inflammatory process.
As a characteristic feature, so-called rheumatic nodules form in up to 20 percent of cases, especially in the area of the elbows and fingers.
The disease often progresses in flares, which means that it makes the joints particularly painful for some time. In addition, there is then also a pronounced feeling of illness.
Overall, the course of rheumatoid arthritis is highly variable. Spontaneous remission (without therapy) can be expected in about 10 percent of patients.
The distinctive feature of this disease is the attack of the inflammatory cells and substances on the articular cartilage and bone. If inflammation continues unchecked, these joint structures are increasingly degraded and the joints are destroyed. The video shows the process of joint damage.
In addition, other organs may be affected in severe cases, e.g.,
- Eyes,
- Heart and pericardium,
- Lungs and pleura,
- Nerves, and
- Blood vessels.
Proper diagnosis at an early stage is important in all rheumatic diseases. This allows the physician to initiate effective therapy to prevent secondary damage.
The diagnosis of rheumatoid arthritis is made
- Based on the symptoms of the disease and
- By means of a rheumatological examination.
The physician is guided by recognized criteria. For example, the American College of Rheumatology (ACR) has provided criteria. They help identify previously unexplained inflammation in multiple joints as rheumatoid arthritis. These include:
- Morning stiffness of the joints,
- Joint inflammation of three or more joint regions,
- Joint inflammation of the finger joints,
- Symmetrical affliction,
- Rheumatoid nodules, rheumatoid factors, and
- Typical radiological changes.
Laboratory tests can identify rheumatoid factors and inflammatory markers. Rheumatoid factors are also found in other diseases, although they have no diagnostic significance. Therefore, they do not prove rheumatoid arthritis but only indicate it.
Laboratory testing is often uncharacteristic in the early stages. However, there is a permanent increase in inflammatory parameters. Rheumatoid factors can be detected in 80 percent of cases. The CCP level is much more accurate for diagnostics.
X-rays are required at the onset and during the progression of the disease to assess the extent of bone damage.
Additional information about the soft tissues of the joint is obtained using an ultrasound, e.g.,
- Joint effusion and
- Thickening of the synovial membrane due to inflammation.
More complex imaging diagnostic procedures are used for specific questions. This includes, for example, magnetic resonance imaging (MRI) in the case of inflammation in the cervical spine.
If the cause is known, a targeted causal therapy could effectively treat the disease or cure it. Unfortunately, the cause of the development of rheumatoid arthritis is still not fully understood.
Thus, a whole spectrum of therapeutic measures is often necessary. They aim to alleviate pain and disease activity and improve prognosis.
A rheumatologist compiles the individual therapy measures according to the patient's individual situation in terms of the disease. In the subsequent period, they review the effectiveness of the therapy in collaboration with the primary care physician.
Drug therapy for rheumatoid arthritis
A number of medications are available to treat rheumatoid arthritis. There are different drug groups and a large number of medications with different efficacy and side effect profiles. Therefore, special experience is needed to adjust the drug therapy.
The most important thing is to adjust the therapy with so-called disease modifying anti-rheumatic drugs (DMARDs). These can prevent the progression of the disease. With the combined use of different DMARDS (known as "combination therapy") and with the development of new drugs, it is possible to halt the progression of the disease process and improve quality of life in more and more patients.
Within drug therapy, physicians distinguish between basic therapy and symptomatic therapy:
Basic therapy has been almost revolutionized in recent years. New DMARDs, called biologic drugs, intervene directly in the inflammatory process of the synovial membrane at different sites. However, effective blocking substrates (antibodies) can now also be used at other points in the inflammatory process. They can be used, for example, against interleukin-1 or against activated inflammatory cells.
The goal of this new biologic therapy is remission of the disease, i.e., conversion of the inflammation to a dormant state. Furthermore, cytostatic drugs such as methotrexate or azathioprine are used.
For symptomatic therapy, nonsteroidal anti-inflammatory drugs such as ibuprofen, diclofenac, and cortisone preparations are available. With all medications, attention must be paid to undesirable side effects. A well-known example is the consequences of long-term cortisone therapy.
Drug therapy at a glance:
- Anti-rheumatic painkillers (nonsteroidal anti-inflammatory drugs): help with inflammatory pain
- Cortisone: rapid effect on the inflammatory response (but problematic in the long term because of side effects)
- DMARDs: help against inflammation and joint destruction in the long term
- Local therapy measures: Cortisone injections into joints, chemical or radiation synovectomy (sclerotherapy of the inflamed synovial membrane)
Diet for rheumatoid arthritis
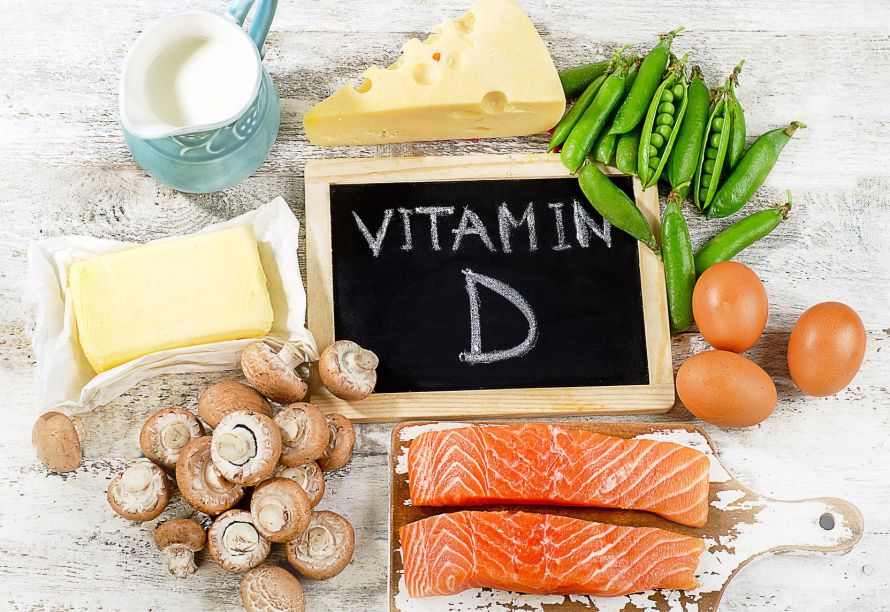
It is also possible to improve symptoms through a suitable diet. For example, a diet rich in calcium and vitamin D can help prevent osteoporosis (bone loss). Unfortunately, the progression of the disease cannot be fundamentally influenced by a change in diet.
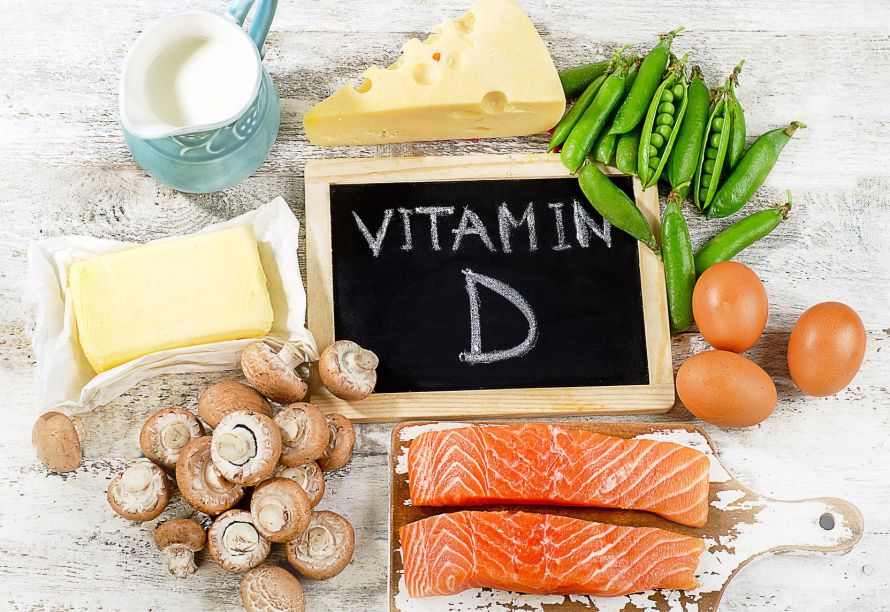
Vitamin D helps prevent rheumatoid arthritis © bit24 / Fotolia
Physical therapy for rheumatoid arthritis
Physical therapy continues to play a significant role alongside medication.
Attention should be paid to appropriate positioning and splinting of the affected limb at an early stage. This helps prevent contractures and joint deformities.
Physiotherapy and occupational therapy play an equally important role in mobilization and muscle care. Applying heat (packs, baths, mud) can be considered mainly during remission and for spa therapy. Patients usually tolerate cold therapy better during a flare.
Deformities and contractures can be functionally treated with suitable splints.
Surgical therapies for rheumatoid arthritis
Early surgical removal of the synovial tissue (synovectomy) can improve the clinical picture by removing the inflammatory pannus and also slowing down further destruction in the affected joint.
Alternatively, or in combination with radiation synovectomy, the proliferating synovial tissue can be suppressed by a radionuclide.
Several surgical reconstructive procedures may be considered in addition to a synovectomy:
- Tendon replacement,
- Joint reconstruction,
- Capsular shift, and
- Nerve solutions
can individually or in combination improve the destroyed joints. In some circumstances, they also counteract the progression of destruction.
Endoprosthesic joint replacement is one of the most successful surgical measures for rheumatic patients. An artificial joint is available today for almost all joints. The application is primarily based on pain, but also on
- The progressive destruction and
- Functional deficits.
Patients with rheumatism often suffer from several areas of joint damage, so a step-by-step plan has to be set up in a special clinic. It should exhaust all possibilities of conservative and surgical therapy.
Important measures for rheumatoid arthritis at a glance
- Physiotherapy: to maintain joint function, muscle strength, and mobility
- Physical therapy: for pain relief, e.g., cold therapy, electrotherapy
- Occupational therapy: how do I relieve my joints, how may I put weight on them, what aids should I use?
Other measures include:
- Orthopedic therapy: Insoles, crutches, splints, surgical measures (e.g., joint prostheses)
- Psychological therapy: For coping with illness and pain
- Socio-medical measures: Job security, retraining, rehabilitation
- Education and information contribute significantly to the success of the therapy
Tips for dealing with the disease
Rheumatoid arthritis is a chronic disease. In addition to changes in the joints and organs of the body, it also affects patients’ mental well-being. Dealing with pain and functional limitations on a daily basis and giving up activities that were once taken for granted are not easy to cope with.
Adjustments in daily life are necessary, both in terms of the person’s professional and family situation. The help of other people must be called upon in order to be able to cope with the disease in everyday life.
Patient education and information from
- Books,
- Information sheets, and
- The internet
can help patients to adjust to the new situation.