Recommended specialists
Article overview
What is an epigastric hernia?
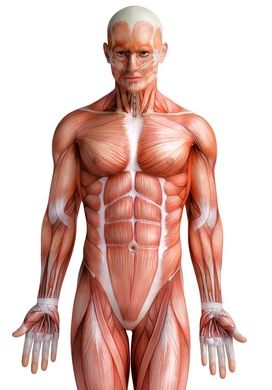
With an epigastric hernia, a gap in the abdominal wall (hernial orifice) appears along the so-called linea alba, i.e. the vertical seam of connective tissue in the middle of the abdomen, which is formed by the fusion of the tendons of the lateral muscles of the abdomen.
© anathomy / Fotolia
Here, parts of the so-called greater omentum, which consists of connective tissue and fatty tissue, and, in rare cases, also parts of the small intestine, protrude outward, forming the contents of the hernia in a sac-like eversion of the peritoneum (hernial sac). Hence, an epigastric hernia is similar to other external hernias such as an inguinal hernia, an incisional hernia or an umbilical hernia.

Hernia with typical spherical protrusion under the skin © Prof. Dr. med. Thomas W. Kraus
Frequency of epigastric hernias
Epigastric hernias occur distinctly less frequently than inguinal hernias or umbilical hernias, for example. So, these represent only approximately 1.6 to 3.6 percent of all abdominal hernias. Those affected are generally middle-aged. Men and women suffer epigastric hernias with approximately equal frequency.
Causes and risk factors for epigastric hernia
An epigastric hernia appears if the abdominal wall is weakened due to a congenital connective tissue weakness and, at the same time, there is increased internal abdominal pressure along the midline of the abdomen. An increase in the internal abdominal pressure can be caused by frequent coughing, for example, due to chronic lung conditions, frequent and intense pressure on defecation due to chronic constipation, for example, and increased carrying of heavy loads, among other things. The risk factors which can favor the appearance of an epigastric hernia also include being overweight, pregnancy and abdominal dropsy (ascites).
Symptoms of epigastric hernia
An epigastric hernia, as a rule, is distinguished by a protrusion along the midline of the upper abdomen between the breast bone and the navel, which is externally visible and/or palpable. The typical symptoms of an epigastric hernia also include the sudden occurrence of severe pain in the upper abdomen, which is caused or exacerbated by an increase in the internal abdominal pressure, such as on coughing, on defecation, or on lifting heavy loads. If the intestine is incarcerated in the hernial orifice due to a large epigastric hernia, together with severe, persistent pain, nausea and vomiting can also occur.
Diagnosis of epigastric hernia
An epigastric hernia is generally diagnosed in the course of detailed history taking and a thorough physical examination. During the history taking, the patient is questioned in detail concerning his medical condition, lifestyle and his medical history. Over the course of the physical examination, the physician palpates the patient’s upper abdomen thoroughly. The physician may possibly already feel the hernial orifice and the protruding hernial sac during this so-called palpation and hence make the diagnosis of an epigastric hernia. Further imaging examinations such as ultrasound examination, computed tomography and magnetic resonance imaging can be also employed subsequently in order to be able to diagnose the epigastric hernia reliably and clearly or to exclude or confirm other conditions.
Treatment of epigastric hernia
Since an epigastric hernia will not recede by itself, the symptoms can deteriorate over time and there is the risk of incarceration of intestine in the hernial orifice, an epigastric hernia should always be surgically treated within the framework of hernia surgery.

Hernia surgery with net © Prof. Dr. med. Thomas W. Kraus
Here, with the closure of the rupture by means of direct suturing (fascia suture) and closure of the rupture by means of the implantation of a synthetic mesh, two surgical techniques are available in principle for the surgical treatment of an epigastric hernia. The procedure can be performed both minimal invasively and in the course of an open procedure. The surgical technique employed depends on the size of the epigastric hernia and the severity of the condition.



























