Recommended specialists
Article overview
Cardiac valve reconstruction - Further information
Valvuloplasty is not necessarily the recommended surgical treatment option for most people who suffer from aortic valve stenosis. However, balloon valvuloplasty might be considered helpful in the case of some children, teens and young adults who suffer from the condition. In this group, it is common for aortic valve stenosis to occur as a result of a congenital heart defect – for example, a bicuspid aortic valve, which has to function with only two valve leaflets, rather than the usual three.
In addition, pregnant women, most older adults and those who are too ill to have immediate aortic valve replacement surgery, may be offered a valvuloplasty procedure as a temporary solution, pending a later, full aortic valve replacement procedure.
Balloon valvuloplasty is usually an effective remedy for aortic valve stenosis in children, teens and young adults. However, most older adults will find that the valve-narrowing problem recurs less than a year after undergoing the procedure.
The reason for this discrepancy is that the effects of ageing create aortic sclerosis as calcium deposits build up and stiffen the valve components, much in the way that plaque deposits gradually harden artery walls. Though defective, the valve structure in a younger person is more flexible and fit for purpose, though even here a certain narrowing may recur, but over a much longer period.
When is valvuloplasty used?
A valvuloplasty can often be used to repair a faulty heart valve.
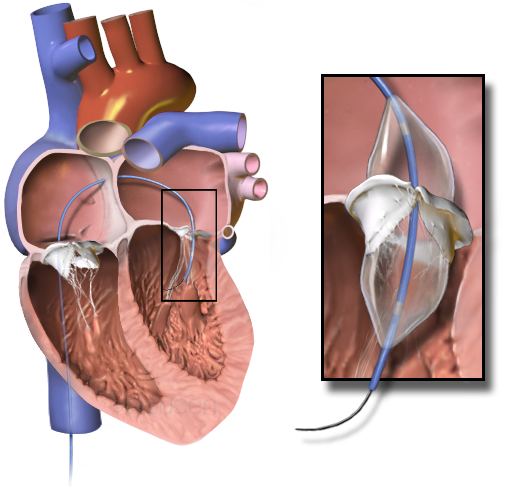
During this procedure, the surgeon will insert a catheter (a long, thin tube) into an artery in the arm or groin. The catheter is equipped with a balloon at its tip and is guided through your vascular system via X-ray imaging. Once the catheter arrives at the location of your heart valve, the tip is inserted into the valve and the surgeon then feeds air into the balloon, causing it to expand. This has the effect of opening the valve, thus separating its leaflets. Once this is achieved, the balloon is deflated and removed along with the catheter.
A valvuloplasty procedure may result in an improved blood supply flowing through your heart, which will reduce your symptoms and discomfort. However, it is possible your valve will narrow once again. This could mean that a valvuloplasty procedure may have to be repeated, or you may need a more permanent solution (such as a valve repair) in future, or even an artificial replacement heart valve.
What are the risks of valvuloplasty?
For children, teens, and young adults, a valvuloplasty carries a low risk of serious complications.
However, where this procedure is used for older adults, there are some risks to consider, including:
- stroke
- heart attack
- aortic valve regurgitation (blood leakage)
Complications related to the use of a catheter include:
- swelling, tenderness and pain at the catheter insertion site
- superficial thrombophlebitis (vein irritation caused by the catheter)
- bleeding and bruising at the catheter site
- temporary urinary problems following the procedure
Are there alternatives to valvuloplasty?
The alternatives to a valvuloplasty procedure include:
- replacement of your natural heart valve with an artificial, mechanical heart valve
- a commissurotomy to separate any valve leaflets that have fused together, thus widening the valve aperture
- decalcification to remove any calcium deposits on the leaflets, which will allow them to open and close more efficiently, thus improving valve functioning
- inserting an annulus support fashioned from tissue or synthetic materials, which will tighten and re-form a valve annulus that has become too wide
- patching heart-valve leaflets, which may have tears or holes that may impair valve performance








