The diaphragm is a dome-shaped muscle that separates the chest cavity from the abdominal cavity. Its main function is to support breathing. If there is a hernial gap in the diaphragm (diaphragmatic hernia or hiatal hernia), organs can slide from the abdominal cavity into the chest cavity through the gap in the diaphragm and may get stuck or incarcerated in the gap. This can for instance lead to intestinal loops dying off.
Recommended specialists
Article overview
Diaphragmatic hernia operation - Further information
Milder complaint symptoms can in some cases be remedied by medication, but if more severe symptoms occur and if there is a risk of organ injuries, a diaphragmatic hernia operation should be carried out. The operation is carried out under general anesthesia. Various methods are available. Today, an instrument-assisted inspection of the abdominal cavity (laparoscopy) is in most cases performed. In this procedure, instruments and a tiny video camera are inserted via small incisions. In some cases, an abdominal incision (laparotomy) may be required though.
Possible causes and risks for diaphragmatic hernia
Although no exact cause of diaphragmatic hernia is known, it can be observed that its frequency increases with age. This allows the conclusion to be drawn that manifestations of wear of the connective tissue in the region of the mouth of the esophagus (at the transition to the stomach) play a role in the development of hiatal hernia.
But the increased occurrence of hernias of the diaphragm is not only associated with increasing age, but also with overweight. This is presumably the case because the pressure on the diaphragm increases due to the overweight, with the possible result that a diaphragmatic hernia may develop. But general weakness of the connective tissue can likewise facilitate the development of a diaphragmatic hernia.
Besides these acquired forms, diaphragmatic hernias can also be congenital, which may necessitate an operation already in early infancy.
If no surgery is performed in the case of a diaphragmatic hernia with complaint symptoms or repeated (recurring) organ displacement, then various difficulties may arise, depending on the type, location and size of the hernia.
In the case of a paraesophageal hernia (located beside the esophagus), displacement of parts of the stomach and the intestine into the chest cavity is possible, even if the stomach has not become completely detached. In this case, a hiatal hernia operation is indicated particularly if there is a risk that parts of the stomach or intestine become incarcerated (get stuck) in the gap, which may lead to disturbances of the blood supply, and even to parts of the intestine dying off and to rupture (perforation) and inflammation of the peritoneum (peritonitis). These complications can be avoided by a hiatal hernia operation performed in a timely manner.
In the case of large diaphragmatic hernias, the function of the heart and lungs may even be impaired because the parts of the stomach and the intestine which are located in the chest cavity may lead to a restriction of the space available for the heart and lungs. In this case, too, a hiatal hernia operation must be carried out. But there are other cases too where a hiatal hernia operation can prevent further damage. In axial hernias, for instance, acidic stomach contents can flow back into the esophagus (reflux disease). In the long run, this may lead to an inflammation of the mucous membrane (reflux esophagitis), which in turn increases the risk of developing cancer in the esophagus (esophageal carcinoma). Here, too, a hiatal hernia operation is the treatment of choice.
Diaphragmatic hernia operation: Preparation and pre-examinations
Depending on where the diaphragmatic hernia is located and how large it is, it may cause no complaint symptoms at all, or it may even develop into a life-threatening inflammation of the peritoneum. It must therefore first be determined precisely, what type of diaphragmatic hernia is present and whether it can be cured by means of an operation. To this end, a physical examination is performed prior to a possible diaphragmatic hernia operation, with particular focus on the examination of the gastrointestinal region. Resistances perceived when pressing-in the abdominal wall during palpation are looked out for, as are unusual bowel sounds.
As soon as a diaphragmatic hernia is suspected, an X-ray image with contrast medium is made. This examination is also known as a barium swallow X-ray. Before having their upper abdomen X-rayed, the patients drink a contrast medium which gets distributed in the stomach and the intestine, so that these organs can be better depicted in the X-ray image. In addition, an instrument-assisted inspection of the esophagus, the stomach and the first part of the intestine (esophagogastroduodenoscopy) is normally performed prior to a diaphragmatic hernia operation. Sometimes, a computed tomography (CT), in which the hernia can be clearly depicted, is also performed prior to a diaphragmatic hernia operation.
Furthermore, a measurement of the function of the esophagus (manometry) and a measurement of the acid content in the esophagus (pH-metry) can be performed. If pronounced inflammations of the esophageal mucous membrane due to the reflux are present which have already persisted for a longer period of time, then tissue samples must be taken in order to rule out malignant changes (tumors). Where applicable, medications that inhibit the blood coagulation (e.g. Marcumar or aspirin) must be discontinued in consultation with the physician prior to the diaphragmatic hernia operation.
Diaphragmatic hernia operation: Procedure and methods
In the diaphragmatic hernia operation (hiatal hernia operation), an instrument-assisted inspection of the abdominal cavity (laparoscopy) is normally used as surgical access. Several methods for diaphragmatic hernia surgery exist, the so-called fundoplication being the most common one. In the fundoplication method, a cuff is formed from portions of the stomach, and this cuff is wrapped around the lower part of the esophagus. This causes a reduction in the backflow of acidic stomach contents into the esophagus (reflux). The chymus or food pulp, on the other hand, can continue to be conveyed into the stomach by the esophagus. This operation is normally carried out in the form of an instrument-assisted inspection of the abdominal cavity (laparoscopy), with small skin incisions being made, via which surgical instruments and a small camera are introduced into the abdominal cavity.
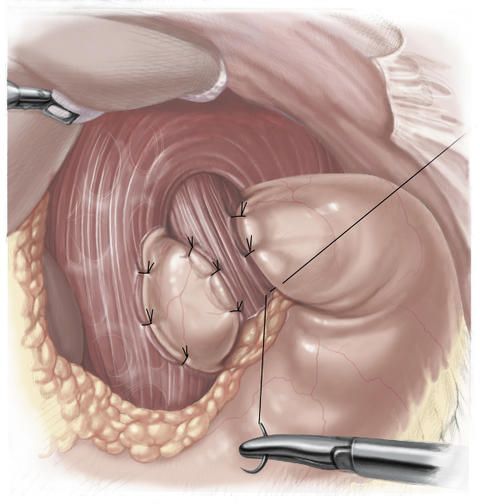
There are two different fundoplication procedures. In the fundoplication procedure according to Nissen and Rosetti, the cuff is wrapped completely around the esophagus by passing the anterior or front wall of the gastric fundus behind the esophagus.
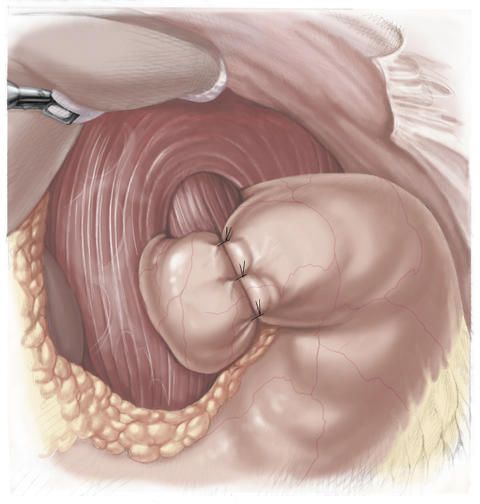
The loop formed in this way is then sutured onto the anterior wall of the stomach. The cuff is additionally attached by sutures to the diaphragm.
In the fundoplication procedure according to Toupet, the loop is not completely wrapped around the esophagus and the cuff is attached with sutures both to the diaphragm and to the anterior wall of the esophagus.
This method is used primarily in patients with movement disorders (motility disorders) of the esophagus. In over 90 percent of the affected persons, fundoplication results in a permanent cure. In this way, particularly young people with reflux disease are spared long-term medication.
Another surgical technique used to treat diaphragmatic hernia is gastropexy, also referred to as fundopexy. In this procedure, the stomach is moved into its normal position and is then sutured onto the anterior abdominal wall so that it can no longer be displaced. In a hiatoplasty (also referred to as hiatal restriction), the diaphragmatic gap is sutured so as to narrow it.
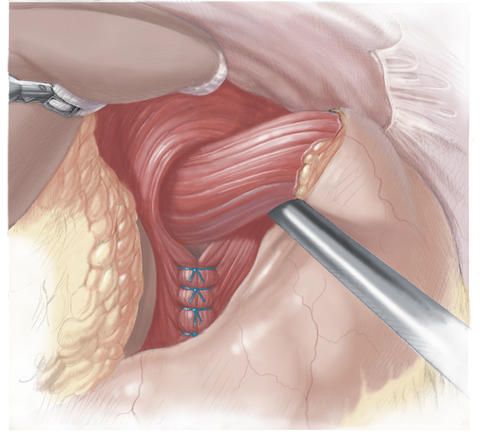
The gap in the diaphragm that has become too large is made smaller so much that only the esophagus will still fit through. The edges of the gap in the diaphragm are then joined again by special sutures. If required, a synthetic mesh is additionally affixed onto these sutures in order to reduce the risk of renewed hernia.
Diaphragmatic hernia operation: Complications and risks
If a diaphragmatic hernia operation (hiatal hernia operation) was necessary, the complaint symptoms in most cases subside completely after the intervention. In rare cases, certain complications may nevertheless arise. It should be pointed out in this context that in centers where diaphragmatic hernia operations are frequently performed, the complications occur less frequently.
The most common complication is the occurrence of flatulence after the diaphragmatic hernia operation. This harmless, though unpleasant, complication is due to the fact that the air from the stomach can no longer get into the esophagus and more air is therefore discharged into the intestine. Less commonly, difficulties in swallowing occur due to the fact that the diaphragmatic hernia operation has resulted in a constriction of the transition between the esophagus and the stomach.
An injury of the vagus nerve (so-called bowel nerve) can also occur in the course of a diaphragmatic hernia operation. This can potentially lead to a stomach emptying disorder. Furthermore, an injury of the phrenic nerve (so-called diaphragmatic nerve) can likewise occur in the course of a diaphragmatic hernia operation. If this nerve is injured, breathing difficulties can result.
And as in any surgical intervention, it cannot be completely ruled out either in the case of a diaphragmatic hernia operation that organs and tissues close to the surgical site are damaged, with the possible result of hemorrhages or post-operative hemorrhages.
Diaphragmatic hernia operation: Post-operative care
For a diaphragmatic hernia operation, an in-hospital stay of around three to five days must be reckoned with. The success of the operation is ensured by means of a renewed X-ray examination with contrast medium, in which particularly the region of the transition from the esophagus into the stomach is once more checked. Since the transition from the esophagus into the stomach is often still somewhat swollen immediately after the diaphragmatic hernia operation, the nutrition during the first few days consists of food of liquid or porridge-like consistency.
It may take a longer period of time until normal stability of the diaphragm is restored. Therefore, activities that involve exposure to too great strain, such as for instance lifting heavy objects or too intense sports, should be refrained from for up to six weeks after the operation.
























