Inguinal hernia, also referred to as groin hernia, is the most common type of hernia, accounting for around 75 to 80 percent of all visceral or bowel hernias. The inguinal hernia operation is therefore the most common hernia operation.
Recommended specialists
Article overview
- What is an inguinal hernia?
- Procedure and methods applied in an inguinal hernia operation
- Inguinal hernia operation according to Shouldice
- Inguinal hernia operation according to Lichtenstein
- Minimally invasive techniques
- TAPP (transabdominal preperitoneal mesh implantation)
- TEP (total extraperitoneal patch-plasty)
Inguinal hernia operation - Further information
What is an inguinal hernia?
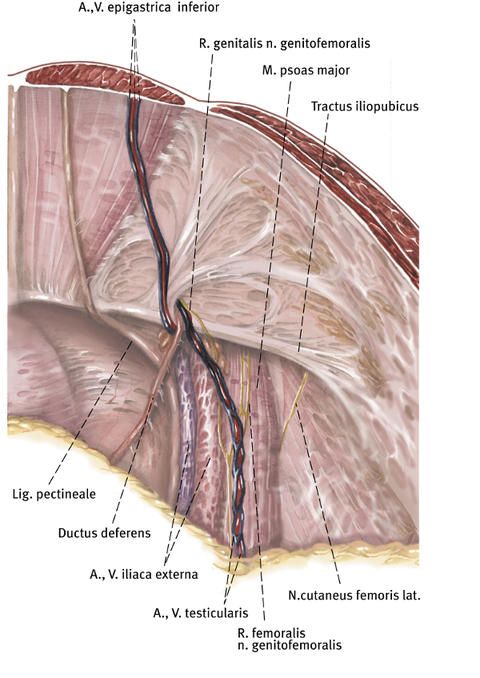
An inguinal hernia is a visceral hernia in the region of the inguinal canal. The inguinal canal runs obliquely through the abdominal wall and is formed by the muscles of the abdomen. In men, the seminal cord, which originates in the testicle, along with its accompanying blood vessels and nerves, passes through the inguinal canal. In women, a thin ligament that holds the uterus passes through the inguinal canal. Men are considerably more frequently affected than women.
If the muscles of the abdomen are weakened, the inguinal canal is dilated and a hernial gap, a so-called inguinal hernia, develops in the abdominal wall. Through this hernial gap, parts of the abdominal organs, such as for instance parts of the intestine, may protrude from the abdominal cavity and become palpable and also visible there as protrusion. This may be associated with pain in the groin region, particularly upon physical exertion, and in the worst case with an incarceration of the abdominal bowels (bowels getting stuck), for example the intestine, in the inguinal canal.
An inguinal hernia is in most cases harmless and often does not cause any discomfort or only mild discomfort. However, since in the case of an inguinal hernia the hernial gap will never close spontaneously, but rather will become larger and larger over time, and there is furthermore a risk that for instance the intestine is incarcerated or gets stuck in the inguinal canal and is cut off from the blood supply, an inguinal hernia should normally be treated by surgical intervention.
Procedure and methods applied in an inguinal hernia operation
Today, many different surgical procedures are available for the surgical treatment of an inguinal hernia. In these procedures, the surgeon displaces the hernial contents back into the abdominal cavity, closes the hernial gap in the abdominal wall and stabilizes the tissue. Which procedure is to be used in an inguinal hernia operation must be decided by the physician and the patient on a case-by-case basis and depends on various factors. Thus, the surgical procedure to be applied in an inguinal hernia operation in a given case depends on the type, location and size of the inguinal hernia and the patient's age and concomitant diseases.
The hernial gap in the abdominal wall can be closed in the scope of an inguinal hernia operation either with pure suture procedures, in which the inguinal hernia is treated and reinforcement is accomplished with sutures, or with procedures in which a synthetic mesh is used. This can be effected either conventionally in the scope of an open intervention, or as minimally invasive surgery using an endoscopic or laparoscopic procedure. Meanwhile, most inguinal hernia operations worldwide are carried out using synthetic mesh implants.
Based on these various surgical options, three different surgical procedures can therefore in principle be applied in an inguinal hernia operation, namely the open surgical technique without synthetic mesh (inguinal hernia operation according to Shouldice), the open surgical technique with synthetic mesh (inguinal hernia operation according to Lichtenstein), and minimally invasive surgical techniques with synthetic mesh (TEP, TAPP).
Inguinal hernia operation according to Shouldice
This inguinal hernia operation method was developed in 1944 by the Canadian surgeon Edward Earle Shouldice. Until the introduction of the surgical procedures in which a synthetic mesh is implanted, this method was considered the gold standard in hernia surgery. The inguinal hernia operation according to Shouldice is a conventional, i.e. non-minimally-invasive operation method in which the hernial gap is closed with the body's own tissue.
The procedure according to Shouldice is as follows: The surgeon makes a transverse skin incision approximately 5 to 8 centimeters long above the inguinal ligament. From this access, he exposes the hernial sac that has formed due to the inguinal hernia.
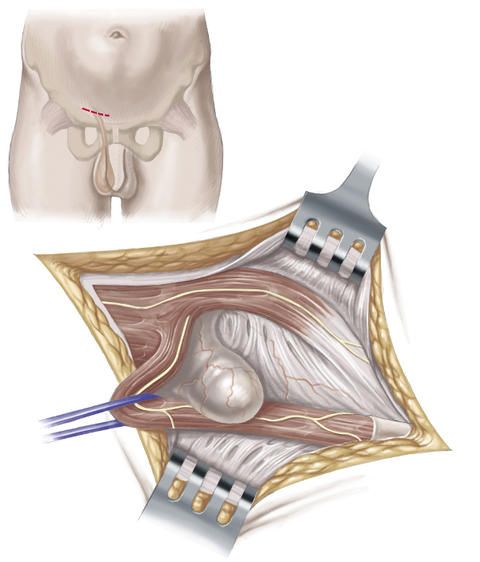
He then opens the hernial sac, checks the bowels that are in the hernial sac, treats them if required and then displaces them back into their original positions in the abdominal cavity. The hernial sac is then removed and the peritoneum is closed with a suture.
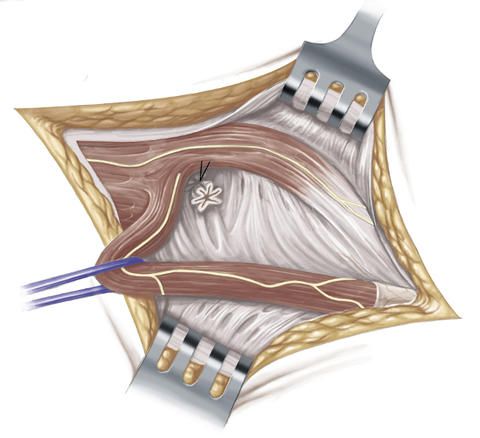
Next, the transversal fascia is opened transversely and mobilized.
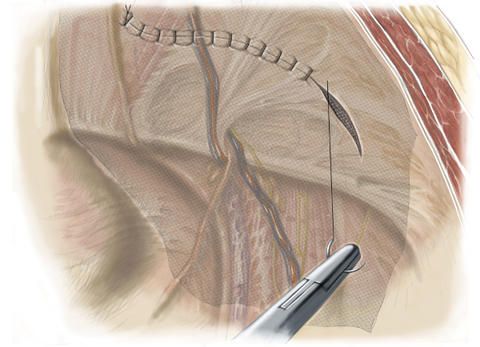
In order to additionally stabilize and reinforce the rear wall of the inguinal canal, the surgeon sutures the inguinal ligament onto the transversal fascia which runs in transverse direction and which constitutes the adjoining connective tissue that lines the inside of the abdominal wall. In order to be on the safe side, this suture is made in several rows.
The inguinal hernia operation according to Shouldice is considered the best suture procedure and features a comparatively low recurrence rate of inguinal hernias that recur after an operation. This type of operation is primarily used for smaller inguinal hernias in young patients without substantial risk profile.
The inguinal hernia operation according to Shouldice is normally carried out in general anesthesia. One of the advantages of this operation method is that the intervention can also be carried out under spinal anesthesia or local anesthesia though. Moreover, this inguinal hernia operation requires no artificial material.
However, patients have to avoid exposure to physical strain for a long time after this open inguinal hernia operation. Thus, they must wait for about two months before they are once more allowed to expose themselves to strain or do sports.
Inguinal hernia operation according to Lichtenstein
This inguinal hernia operation method was developed in 1984 by the American surgeon Irving Lester Lichtenstein and meanwhile has become one of the most commonly used surgical procedures for the treatment of an inguinal hernia. As in the case of the inguinal hernia operation according to Shouldice, the inguinal hernia operation according to Lichtenstein is an open, i.e. non-minimally-invasive surgical procedure. In contrast to the inguinal hernia operation according to Shouldice, the hernial gap, in the Lichtenstein method, is not closed with the body's own tissue though, but rather with a special synthetic mesh.
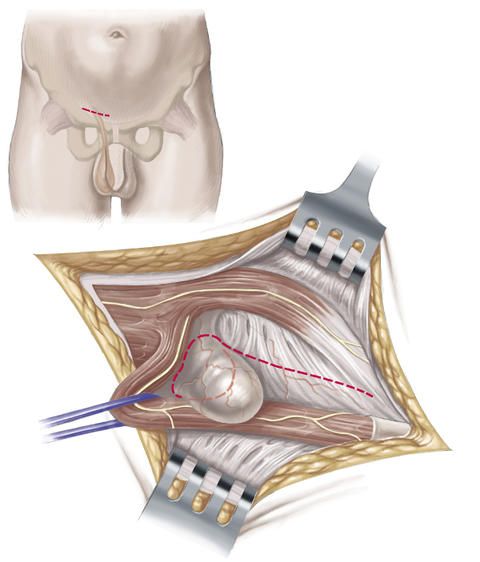
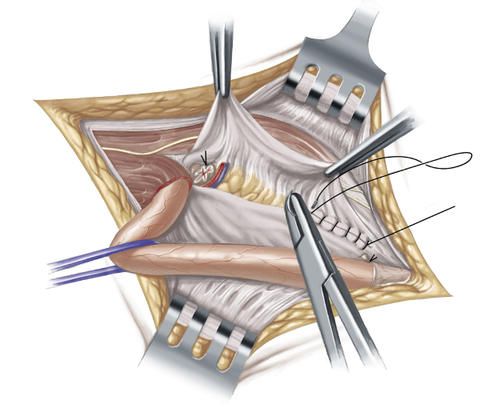
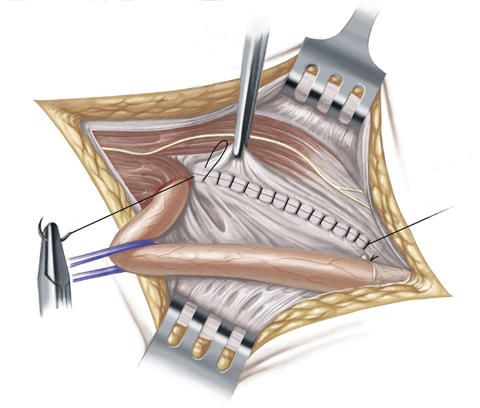
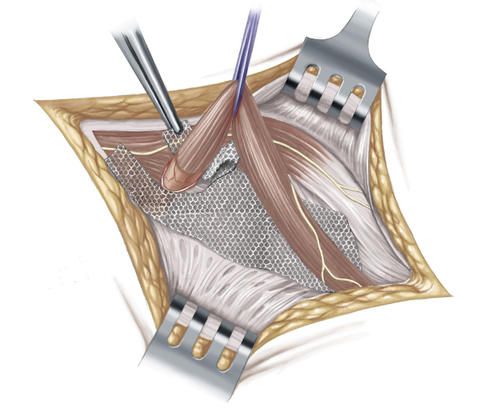
At first, the inguinal hernia operation according to Lichtenstein proceeds in the same way in principle as the inguinal hernia operation according to the Shouldice method: The surgeon makes a transverse skin incision approximately 5 to 8 centimeters long above the inguinal ligament and then exposes the hernial sac and opens it. The contents of the hernial sac are pushed back into the abdominal cavity, the hernial sac is removed and the peritoneum is closed with a suture. But in the next step, the surgeon, in contrast to the Shouldice method, covers the hernial orifice with a thin synthetic mesh made of polypropylene and affixes this with sutures to the muscles of the abdominal wall and to the inguinal ligament.
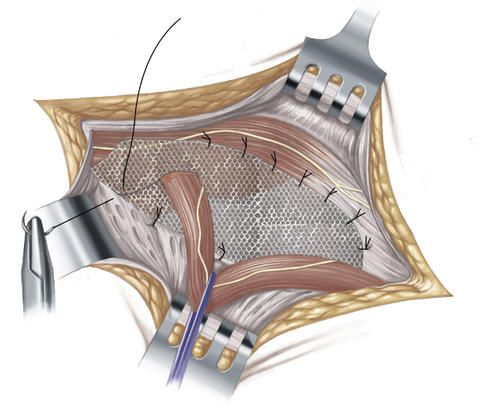
The inguinal hernia operation according to Lichtenstein is suitable particularly for elderly people and for patients with a medium-sized or large inguinal hernia. Furthermore, this operation method is also used in patients who have suffered a recurrence of the inguinal hernia (recurrent hernia).
An advantage of the Lichtenstein method is that the intervention can also be carried out under spinal anesthesia or local anesthesia and does not necessarily require general anesthesia. The risk of recurrence of an inguinal hernia after the operation is low. Moreover, after the inguinal hernia operation according to Lichtenstein, the patients are allowed to once more expose themselves to physical strain at an earlier stage and are once again physically fit faster than after a Shouldice operation.
Minimally invasive techniques
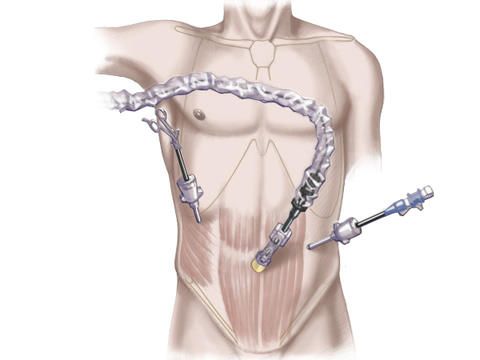
In contrast to the open procedures according to Shouldice and Lichtenstein, a minimally invasive inguinal hernia operation does not require a large skin incision in the inguinal region, but rather is carried out by means of small abdominal incisions below the navel, through which an endoscope as well as the required surgical instruments are introduced and advanced up to the inguinal hernia. Minimally invasive surgical procedures are therefore also referred to as keyhole surgery.
With the so-called TAPP (transabdominal preperitoneal hernioplasty) and the so-called TEP (total extraperitoneal hernioplasty), two different variants of a minimally invasive inguinal hernia operation are available. Both procedures use large-area synthetic meshes which are implanted from the rear side of the abdominal wall, and both are always performed in general anesthesia.
One of the advantages of a minimally invasive inguinal hernia operation is that the patient is already allowed to expose himself to physical strain again after a few days. Furthermore, the synthetic mesh is placed loosely over the inguinal hernia without the latter having to be closed with sutures under tension. As a result, the patient normally feels no dragging pain after the operation and is more quickly mobile again. The minimally invasive inguinal hernia operation is carried out under general anesthesia.
The minimally invasive techniques can in principle be applied in all patients in whom no contraindications are present. They are also used in repeat interventions in which the surgical access from outside is rendered more difficult due to a previous inguinal hernia operation.
TAPP (transabdominal preperitoneal mesh implantation)
For the minimally invasive inguinal hernia operation by means of TAPP, the procedure is as follows: The surgeon makes small incisions in the region of the navel and in the mid-abdominal region. He then introduces a special needle via which he fills and inflates the abdomen with carbon dioxide. This serves to push back the intestine and enable the surgeon to have a good view of the inguinal hernia to be operated on. In the next step, he introduces the endoscope with the camera and the surgical instruments via the skin incisions.
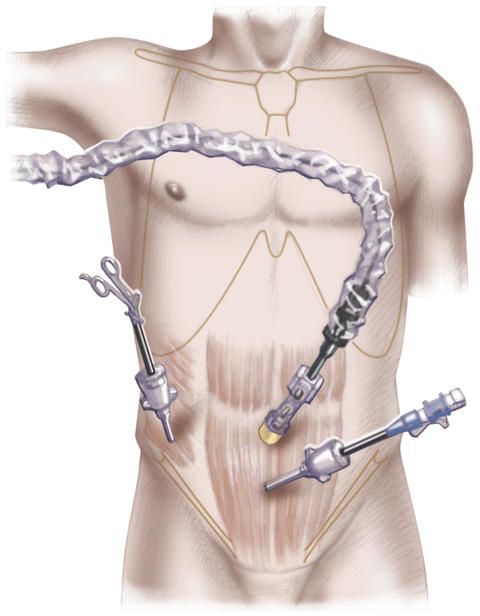
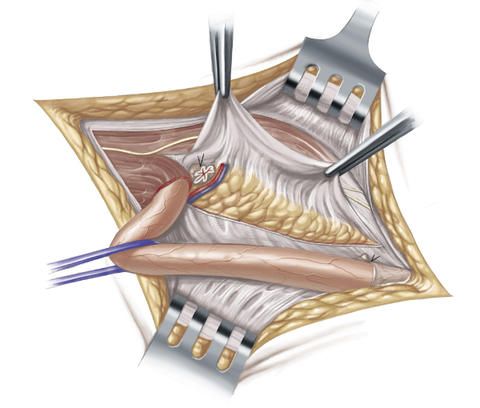
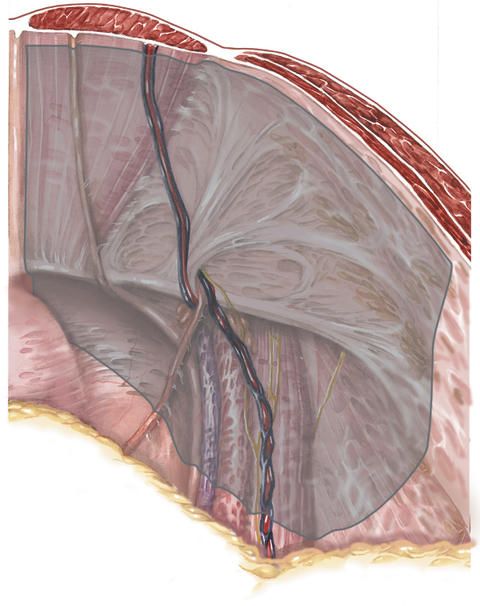
An incision is now made into the peritoneum, the hernial sac is carefully detached from the hernial orifice and the hernial contents are pushed back into the peritoneal cavity.
A sufficiently large synthetic mesh is advanced from the abdominal cavity (transabdominally) up to the inguinal hernia and is then placed over the hernial orifice before the peritoneum (preperitoneally).
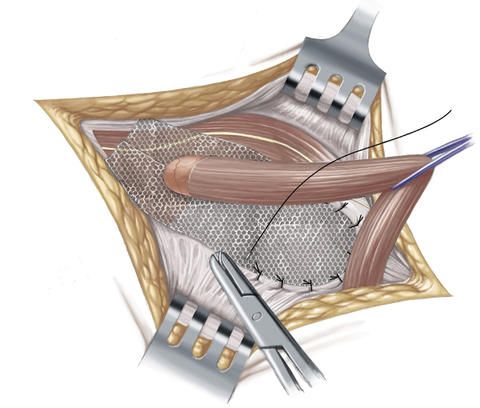
The synthetic mesh is normally at least 15 x 10 centimeters in size and is fixed in place with the aid of glue, or holds without fixation. The opening in the peritoneum is closed with a suture in order to prevent the synthetic mesh from coming directly into contact with the intestinal loops.
In the case of a bilateral inguinal hernia, both hernias can be treated in a single intervention with the TAPP method. The TAPP procedure is therefore used particularly also in cases of bilateral inguinal hernia. Furthermore, it is often carried out in cases of repeated inguinal hernia (recurrent hernias) that have already been treated in a previous open operation.
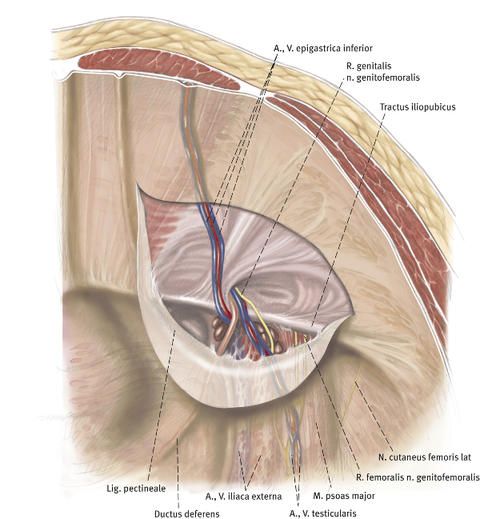
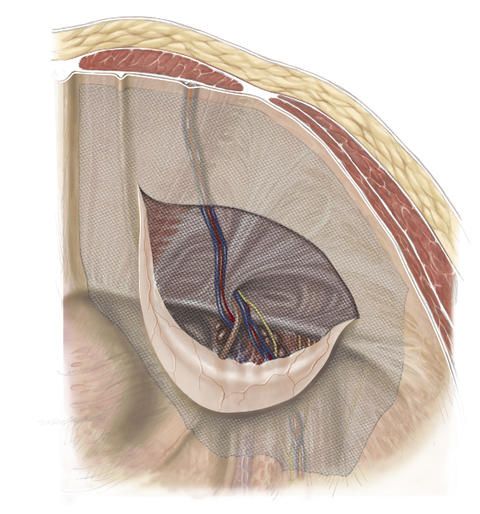
TEP (total extraperitoneal patch-plasty)
In the inguinal hernia operation by means of TEP, the peritoneal cavity is not opened up. Surgery is performed in the so-called preperitoneal space before the abdominal wall. The risk of injuring inner organs such as the intestine is therefore even lower. The procedure for the minimally invasive inguinal hernia operation by means of TEP is as follows: The surgeon makes a small skin incision below the navel, and then inserts an air-filled balloon between the abdominal wall and the peritoneum via this incision.
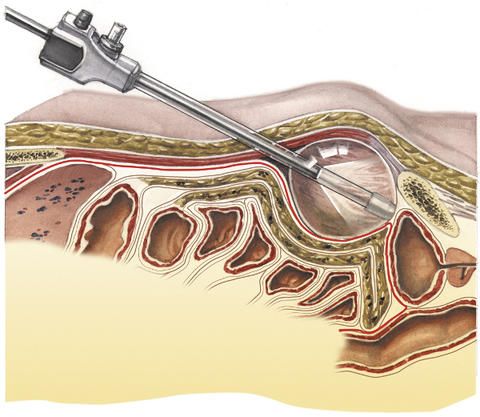
This serves to detach the abdominal wall from the peritoneum. In order to widen the gap between these two layers which has been produced in this way, carbon dioxide is then blown into the balloon. The surgeon now has a good view of the area to be operated on.
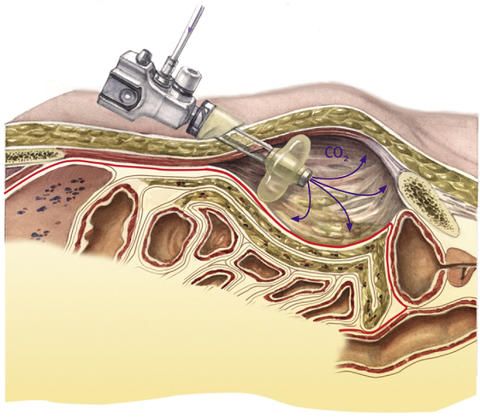
The surgical instruments and the endoscope with the camera are introduced via two additional skin incisions.
The hernial sac is now carefully exposed and the hernial contents are displaced back into the abdominal cavity.
A synthetic mesh is then affixed over the hernial orifice between the abdominal wall layers, i.e. behind the muscle layer and on the peritoneum. This mesh normally fixes itself in place automatically through the natural pressure prevailing in the abdomen and the counterpressure of the abdominal muscles.
Additional fixation by means of tissue glue is therefore in most cases not necessary, but can nevertheless be carried out where necessary.



























