Bone marrow edema (BME) syndrome is characterized by severe, usually load-dependent pain in the affected bone section. Bone marrow edemas most commonly occur in the hip joint, and less commonly in the knee. Possible causes of the disease are circulatory disorders as well as mechanical overexertion or trauma to the bone.
Here you can find additional information and qualified specialists and centers for the treatment of bone marrow edemas.Recommended specialists
Brief overview:
- What is a bone marrow edema? An increased accumulation of water in the bone that causes severe pain, usually related to putting weight on the bone. It occurs most frequently in the hip joint or knee.
- Causes: Circulatory disorders in the bone, mechanical overload with microfractures, comorbidities with other bone and joint diseases.
- Symptoms: Severe pain in the affected bone section, other symptoms are rare. The pain subsides when lying down or sitting.
- Diagnosis: The diagnosis is made by ruling out other diseases and confirming the findings with an MRI.
- Treatment: The underlying condition must be treated, therefore diagnosing the cause is very important. Often, only surgical or palliative care options remain after a late diagnosis.
- Prognosis: The outcome cannot be predicted. It is either a self-limiting disease or a disease that progresses with irreversible bone death.
Article overview
Definition and history of bone marrow edema syndrome
Bone marrow edema syndrome is usually accompanied by severe, often load-dependent pain in the affected bone section. Bone marrow edema, i.e., an increased accumulation of water in the bone, is characteristic of the disease.
The term bone marrow edema syndrome describes the entire complex of
- Cause,
- Pain, and
- Outcome.
In principle, the disease can occur in all bones, but occurs most frequently in the hip joint and less frequently in the knee.
Bone marrow edema syndrome was first described by Curtiss and Kincaid in 1959. At that time, the authors reported on a woman in the last trimester of her pregnancy. She exhibited a clinical syndrome with hip pain and reduced bone density on the X-ray.
The pain syndrome was associated with a transient decrease in radiopacity in the corresponding bone areas. Therefore, Hunter and Kelly named the syndrome "transient osteoporosis" in 1968.
The term bone marrow edema was introduced only after magnetic resonance imaging (MRI) had found its way into the diagnosis of unclear bone and joint diseases. Wilson therefore replaced the term transient osteoporosis with the term transient bone marrow edema syndrome in 1988.
A year later in 1989, Turner reported that this syndrome can be associated with avascular bone necrosis. Since then, many authors have assumed a disease continuum that begins with bone marrow edema and may end in avascular bone necrosis.
Bone marrow edema likely represents an early reversible phase of avascular bone necrosis. This hypothesis is based on similarities in the fine tissue examination of bone, which is identical in both early avascular necrosis and bone marrow edema. According to the Association Research Circulation Osseous (ARCO), four stages can be classified:
- Stage I: Bone marrow edema
- Stage II: Osteonecrosis with focal osteoporosis in X-rays
- Stage III: Subchondral fracture with crescent sign in X-rays
- Stage IV: Collapse of the cortical bone and development of osteoarthritis.
Symptoms of bone marrow edema syndrome
The disease is usually accompanied by severe pain in the affected bone sections. Apart from the pain mostly due to putting weight on the affected area, few other symptoms are found.
The clinical progression of the disease is characterized by position or load-dependent pain. The symptoms improve when lying or sitting. Immobilization or resting the extremity does not result in permanent improvement. Even medication cannot eliminate the pain in the long term.
Diagnosis of bone marrow edema syndrome
Transient osteoporosis may be suspected if four of the five items apply:
- Load-dependent pain,
- Lack of other symptoms,
- No spontaneous improvement,
- No clear improvement from pain medication, and
- Normal X-ray.
Bone marrow edema is not visible on plain X-rays. Only in the later progression is there a temporary decrease in radiopacity in the affected bone section. Indications of transient osteoporosis can be obtained by a bone scintigraphy (or bone scan).
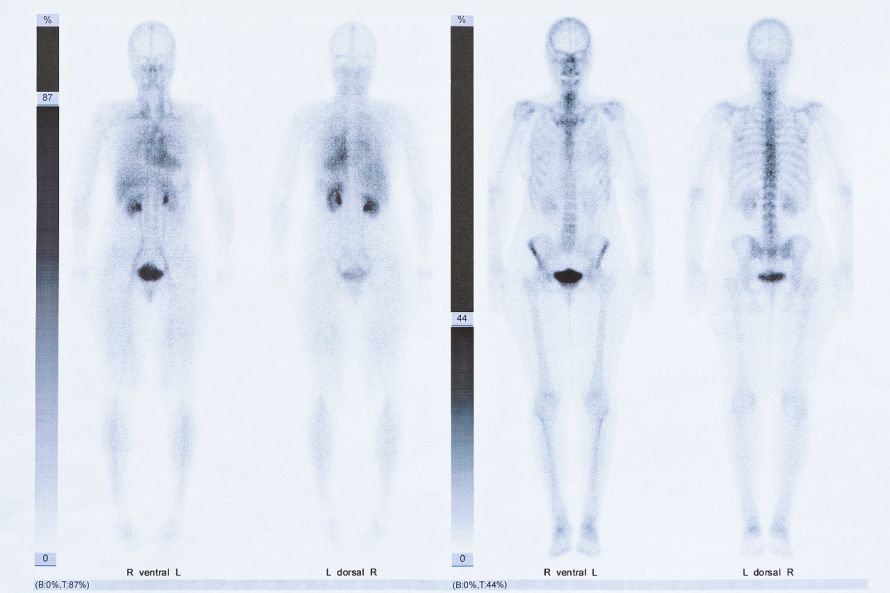
Bone scintigraphy imaging © agenturfotografin | AdobeStock
Bone marrow edema is diagnosed almost exclusively by magnetic resonance imaging. This shows hyperintense staining in STIR and T2 images and hypointense staining of the bone marrow in T1 weighted MRI images.
The disease most commonly occurs in the hip joint, and less commonly in the knee. However, like avascular bone necrosis, it can occur in principle in all bones.
Causes of bone marrow edema syndrome
The syndrome can occur in three situations:
- Circulatory disorder of the bone,
- Mechanical overloading of the bone with microfractures, and
- Reactive comorbidities in other bone and joint diseases.
The circulatory disorder may be caused either by impairment of arterial inflow or venous outflow. The arteries rarely show wall changes or thrombus formations in the biopsies. Therefore, the syndrome is probably more often caused by venous stasis than by arterial interruption of blood supply.
Mechanical bone marrow edema is caused by overloading the bone or by trauma.
Reactive bone marrow edema is associated with, e.g.,
- Osteoarthritis,
- Rheumatism,
- Osteomyelitis,
- Tumors, and
- Bone surgery.
In summary, the following disorders and situations can trigger a bone marrow edema:
- Blood clotting disorders (e.g., thrombophilia),
- Metabolic diseases (e.g., Gaucher's disease),
- Blood disorders (e.g., sickle cell anemia),
- Medication (e.g., cortisone),
- Transplantation (e.g., cyclosporine),
- Pregnancy,
- Sports (e.g., diving),
- Rheumatism (e.g., rheumatoid arthritis),
- Hormonal disorders (e.g., hypogonadism),
- Complex regional pain syndrome (e.g., Sudeck's atrophy.
Treating bone marrow edema syndrome
Therapeutically, the underlying disorder must be treated. Clarifying the cause is therefore essential. Depending on the cause and stage, various forms of therapy are then available.
After a fracture and osteoarthritis occur, the only option is often joint replacement with an endoprosthesis. This surgery is performed by orthopedists.
Often, the syndrome is not correctly diagnosed until the disease progresses. Then only surgical or even palliative care is possible.
Early detection of the disease and clarification of causes allows medical intervention in the various aspects of the disease development. In this way, the progression of the disease can be favorably influenced.
Prospects for curing bone marrow edema syndrome
Transient osteoporosis is
- Either a self-limiting disease or
- It progresses with irreversible bone necrosis.
Currently, there is no way to predict in advance how the disease will progress. In most cases, the disease lasts for about a year.


















