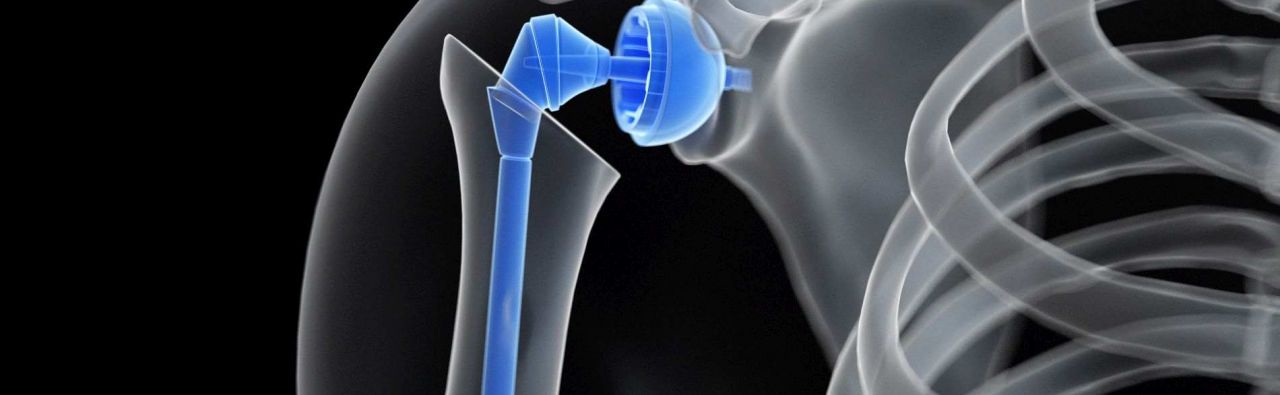
Shoulder endoprosthetics means the complete or partial replacement of the shoulder joint with artificial materials. If the joint is completely replaced, i.e. the acetabulum of the shoulder blade and the head of the humerus, it is also referred to as a shoulder TEP (total shoulder endoprosthesis), if only one joint partner is replaced, it is a hemiprosthesis.
Recommended specialists
Article overview
- What is shoulder endoprosthetics?
- What diseases are treated by shoulder endoprosthetics specialists?
- Which diagnostic methods are used by specialists in shoulder endoprosthetics?
- Which treatment methods belong to the range of services of a specialist for shoulder endoprosthetics?
- What distinguishes shoulder endoprosthetics specialists?
- References
Shoulder endoprosthetics - Further information
What is shoulder endoprosthetics?
The shoulder consists of several joints, the bones of the shoulder girdle and the head of the humerus, as well as the ligaments and muscles surrounding the bones. The largest joint, the shoulder joint, is made up of the humeral head (humeral bone head) and a part of the shoulder blade (the acetabulum). As a ball joint, it is the most mobile joint in the human body. Ligaments and above all muscles serve to stabilize and move the joint.
These muscles are arranged like cuffs around the shoulder joint and are therefore called rotator cuff. Although the mobility is somewhat restricted by other parts and extensions of the shoulder blade, it can still dislocate relatively easily due to the high mobility of the joint (shoulder dislocation). These bony appendages can also break due to external forces and tear the muscles and tendons of the rotator cuff.
The shoulder endoprostheses, which are very well tolerated by the body, consist of a titanium or chromium-chromium alloy and are anchored securely in the bone with or without bone cement (a special plastic), depending on the condition of the bone and the age of the patient.
What diseases are treated by shoulder endoprosthetics specialists?
Shoulder injuries in the past, as a result of rheumatic diseases (rheumatoid arthritis) or other degenerative (wear-related) processes can lead to arthrosis, i.e. joint wear, in the shoulder joint, in which initially the cartilage and, in an advanced stage, the bone itself is broken down. This omarthrosis mainly affects the head of the humerus, but can also occur in the acetabulum and is the most common reason for the implantation of an artificial shoulder joint.
Another relatively common reason for a shoulder endoprosthesis surgery are complex fractures of the upper section of the humerus.
Other diseases or conditions treated by shoulder endoprosthetics experts include, for example:
- humerus head necrosis, i.e. the bone tissue dies as a result of an accident or a disease
- Tumors of the upper segment of the humerus (humerus tumors)
- Rotator cuff defects (rotator cuff arthropathy defect)
- Pseudarthrosis (also referred to as false joint and pseudo joint) of the upper section of the humerus bone (non-healing bone fracture)
- Renewed fracture of an already healed fracture (osteosynthesis)
- Hooked shoulder joint luxation (dislocated shoulder joint)
- Omarthrosis as a result of infection
- Impingement syndrome: pain and limited mobility due to wear and tear or pinching of soft tissue
Which diagnostic methods are used by specialists in shoulder endoprosthetics?
The patient interview (anamnesis), for example, about the type and duration of the symptoms as well as a physical and clinical examination form the basis of the diagnostics. In many cases, this can be used to identify possible causes of the patient's complaints.
However, imaging examinations are indispensable. X-rays play an important role in this process. They can be used to detect fractures and bony changes. Computed tomography (CT) can be used to assess the bone structure, among other things. Soft tissue such as the rotator cuff, bursa and other muscles can be visualized using magnetic resonance imaging (MRI). For a better representation of the joint space, a contrast agent is occasionally injected directly into the shoulder joint and then an MRI is performed (so-called MR arthrography). Ultrasound examination (sonography) and other procedures are also used for certain issues.
Which treatment methods belong to the range of services of a specialist for shoulder endoprosthetics?
The range of services offered by a specialist in shoulder endoprosthetics includes the following methods:
- Implantation of anatomical shoulder prostheses - i.e. the round part of the endoprosthesis is inserted instead of the head of the humerus.
- Implantation of inverse shoulder prostheses - i.e. the round part of the endoprosthesis is inserted instead of the acetabular cup
- Replacement of the humeral head in omarthrosis and after injuries
- Replacement of the humeral head and the acetabulum in omarthrosis and after injuries
- Endoprosthesis in omarthrosis and damage to the rotator cuff
- Inserting special shoulder prostheses, such as the shaft-free shoulder prosthesis or the surface substitute
- Revision (correction) and replacement of shoulder prostheses
- Treatment of complex fractures of the humeral bone head
- Treatment of long-term consequences of humeral head fractures
What distinguishes shoulder endoprosthetics specialists?
Experts in shoulder endoprosthetics are usually specialists in orthopedics, trauma surgery, sports medicine or orthopedic surgery who have particular experience in the field of implanting shoulder endoprostheses. When deciding for or against a surgery, they weigh up the opportunities and risks against each other and consider possible alternatives for an endoprosthesis. Through certification, they guarantee high quality in surgical care.
References
- Deutsche Gesellschaft für Orthopädie und Orthopädische Chirurgie(DGOOC) (2017) S2e-Leitlinie „Rotatorenmanschette“. AWMF-Leitlinien-Register Nr. 033/041
- Deutsche Gesellschaft für Unfallchirurgie e.V. (DGU) et al. (2017) Oberarmkopffraktur. Leitlinien Unfallchirurgie. AWMF-Leitlinien-Register Nr. 012/023
- Garving C, Jakob S, Bauer I et al. (2017) Impingementsyndrom der Schulter. Dtsch Arztebl Int 114(45): 765-76. doi: 10.3238/arztebl.2017.0765
- Jerosch J, Heisel J (2003) Schulterendoprothetik: eine Standortbestimmung – Implantation bei Omarthrosen und Frakturen des proximalen Humerus. Dtsch Arztebl 100(37): A-2366 / B-1978 / C-1865
- Schünke M et al. (2018) Prometheus. Allgemeine Anatomie und Bewegungssystem: LernAtlas der Anatomie. Thieme, Stuttgart