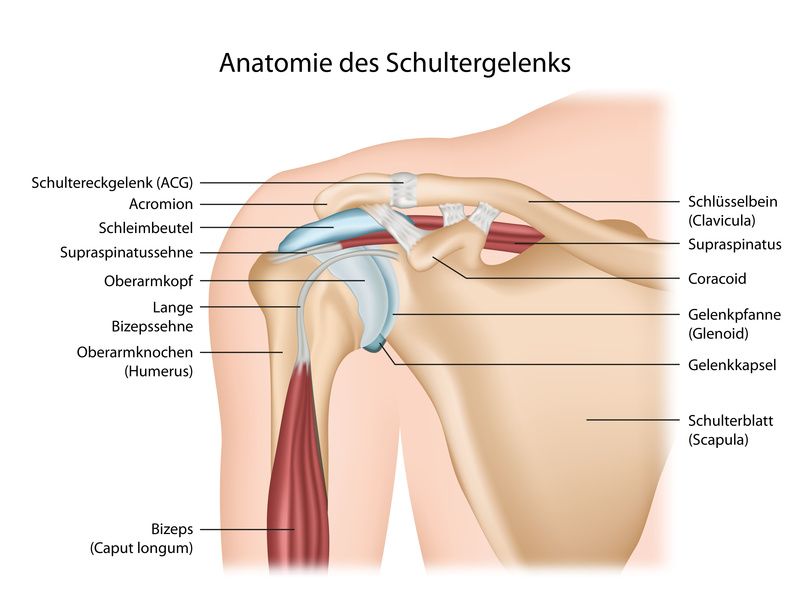
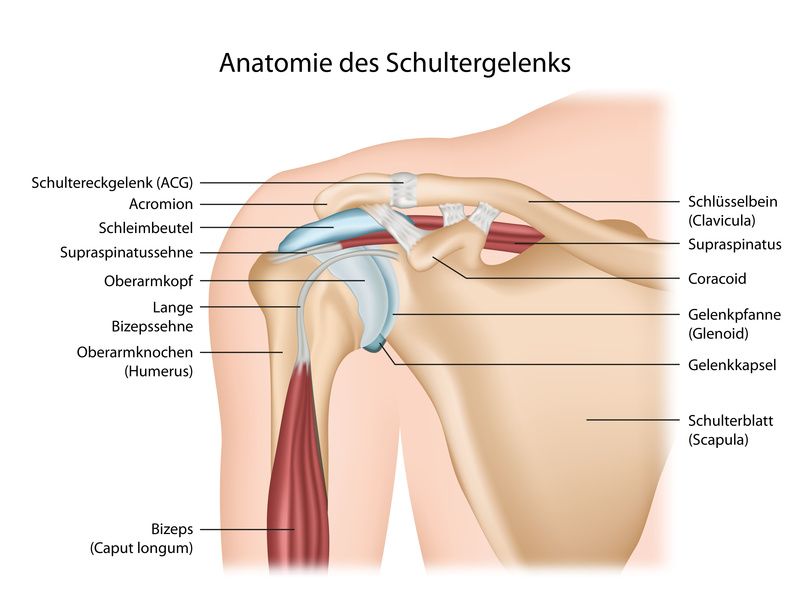
Bursae play an important role in the mobility of our joints. The cushion-like bursa are filled with a gel-like tissue fluid and have a lubricant layer on the surface.
Bursae are located wherever hard structures meet soft structures, for example between bone and tendon. There they act as a kind of damper and prevent the two components from rubbing against each other when they move.
In this way, bursae ensure that the joint can move without friction loss and remains supple.

All joints in the body are protected by bursae. © freshidea / Fotolia
The shoulder joint is exposed to constant stress and is therefore vulnerable © bilderzwerg / Fotolia
Bursae can become inflamed, this is called bursitis. In the case of subacromial bursitis (bursitis of the shoulder, ICD code: M75.5) typical signs of inflammation are shown:
The affected area is slightly to markedly swollen and reacts painfully when pressure is applied. In addition, the skin is usually reddened and feels warm.
The swelling of the bursa severely restricts the range of motion of the tendon. Therefore, the slightest movement of the arm often causes severe pain.
In most cases, this also severely restricts movement in the shoulder joint.
Most often, bursitis in the shoulder area is caused by overloading the shoulder joint. The reason is usually unaccustomed continuous stimulus. During certain activities, the joint makes this arm movement countless times, for example when painting a wall. As a result, tendons and bones keep sliding along the protective bursa pads.
The constant rubbing causes irritation of the bursa surface. This often results in an acute inflammation. If the strain continues, it can develop into chronic bursitis.
One-sided strain, in which a muscle constantly exerts pressure on the bursa can also promote bursitis.
Furthermore a
- shoulder bruise,
- bump or
- fall
can cause subacromial bursitis. In rare cases, a bacterial infection is also to blame for bursitis in the shoulder area.
Bursitis in the shoulder usually occurs in middle-aged people. Certain underlying diseases such as
increase the risk of getting bursitis.
Bursitis in the shoulder usually heals on its own after a few days. However, you must hardly move the shoulder joint for at least three days. It is best to immobilise the arm completely with a sling.
If you continue to put weight on the shoulder joint despite the existing inflammation, the inflammation will probably not improve. There is then a risk that the bursitis will become chronic.
First aid if you have bursitis
As a first measure, it is recommended to cool the shoulder with ice. Cooling counteracts the swelling and relieves the discomfort. However, never place the cooling pad directly on the skin – otherwise there is a risk of freezing. Cooling gels and ointments from the pharmacy also serve their purpose.
Painkillers such as paracetamol help with pain. At first, it makes sense to take a break from exercise until the first pain subsides.

Cooling, pain relief and rest: first aid for bursitis © Microgen | AdobeStock
After a few days, pain and the inflammatory process usually gradually subside. Then it is time to carefully mobilise the shoulder again with special exercises. This is because joints stiffen more quickly than expected if they are not in motion for too long.
To do this, take hold of the affected arm and lead it upwards, outwards and to the centre of the body in three different exercise groups respectively. Perform the movement in such a way that you reach the pain threshold but do not go beyond it. Hold this position for a few seconds.
Repeat each exercise session several times a day 5 - 10 times.
If, despite immobilisation of the affected arm, there is no clear improvement in the symptoms after 4 - 5 days, please consult a doctor. The doctor will usually first prescribe anti-inflammatory medication to stop the inflammatory process in the shoulder.
Another treatment option is cortisone steroid injections. The doctor injects it directly into the shoulder joint or the bursa. This often leads to a rapid improvement of the symptoms.
Doctors usually recommend additional physiotherapy. It makes the shoulder joint fully mobile again.
Rarely, extensive fluid deposits accumulate in the bursa as a result of the inflammation. They lead to an easily palpable swelling. If these do not regress by themselves in the course of healing, cannulation is necessary. During this procedure, the doctor draws off the stored tissue fluid with a thin cannula.
Older people in particular are advised to see a doctor if they suspect they have bursitis.
The first thing to do is to distinguish bursitis from other possible diseases. Arthrosis, rheumatism or gout are also accompanied by similar symptoms.
In case of doubt, the doctor will perform an ultrasound examination (sonography) or X-ray. If the result is inconclusive, the doctor may take an additional blood and urine test.
Sometimes bursitis can persist after 3 - 6 weeks despite medical treatment. Then the doctor considers a surgical intervention. Bacterial bursitis also sometimes requires surgical intervention.
During the operation, the surgeon removes part of the bursa and smooths the surface of the bone if necessary. The procedure is performed in an open surgery or minimally invasive with keyhole technique. The healing process is much faster with minimally invasive surgery.
You can prevent overloading of the shoulder joint yourself. A new activity or hobby is often associated with new movements that the body is not used to.
In sports like tennis or rowing, we perform the same movement over and over again for hours. If these repetitive movements are unfamiliar to us, it puts an enormous strain on the shoulder joints.
Here it is advisable not to overstrain the joints. If possible, always take a break for a few minutes. Only in this way does the body have the chance to slowly get used to new movement patterns and to survive stress without damage.
Regular compensatory exercise that keeps the joints fit also reduces the risk of developing bursitis.
People who move little in everyday life are most susceptible to bursitis. Rusty, immobile joints become inflamed particularly quickly when subjected to new, unaccustomed stresses.