Here you can find additional information and recommended specialists and centers for the treatment of fatty liver disease.
Here you can find additional information and recommended specialists and centers for the treatment of fatty liver disease.
Recommended specialists
Brief overview:
- What is a fatty liver disease? A pathological change in the liver that can later turn into liver cirrhosis or liver cancer.
- Frequency: It is a common liver disease in industrialized countries, estimated to affect at least 20-30% of the population.
- Causes: Excessive alcohol consumption, metabolic syndrome (obesity, type 2 diabetes, and elevated blood lipid levels), dyslipidemia, other pre-existing conditions, and medication use.
- Symptoms: With increasing fatty accumulation of the liver, nonspecific symptoms may occur, such as mild pain, a feeling of pressure in the upper right abdomen, and others.
- Diagnosis: Medical history, physical exam, blood test, and ultrasound. In case of suspicion, an elastography and a liver biopsy are performed.
- Treatment: Fatty liver disease is merely a symptom of a pre-existing condition. If this is treated, fatty liver disease can also be controlled.
- Prognosis: The prognosis is usually good if the causes are eliminated as quickly as possible.
Article overview
Definition: What is a fatty liver disease?
Fatty liver disease (also known as hepatic steatosis) is a pathological change in the liver. It occurs when the body makes or receives more fats from outside than it can break down or remove from the liver.
Certain fats (triglycerides) are then increasingly deposited in the liver tissue, leading to a gradual accumulation of fat in the liver cells (hepatocytes). This excess of fat in the liver is also referred to by physicians as hepatic steatosis.
The transition from a healthy liver to a fatty liver is fluid. Doctors speak of a fatty liver disease only if
- More than 50 percent of the liver cells have fatty deposits or
- The percentage by weight of fats in the liver is more than 10 percent of the total weight of the liver.
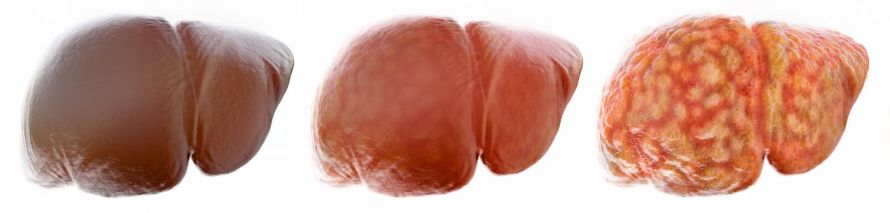
Transition from a healthy liver to a fatty liver © crevis | AdobeStock
Depending on the extent of fatty liver disease, physicians distinguish between three different degrees of severity:
- Grade 1: mild fatty liver disease
- Grade 2: moderate fatty liver disease
- Grade 3: severe fatty liver disease
In addition, a distinction is made between two different forms of fatty liver disease, depending on the cause:
- Alcoholic liver disease and
- Non-alcoholic fatty liver disease.
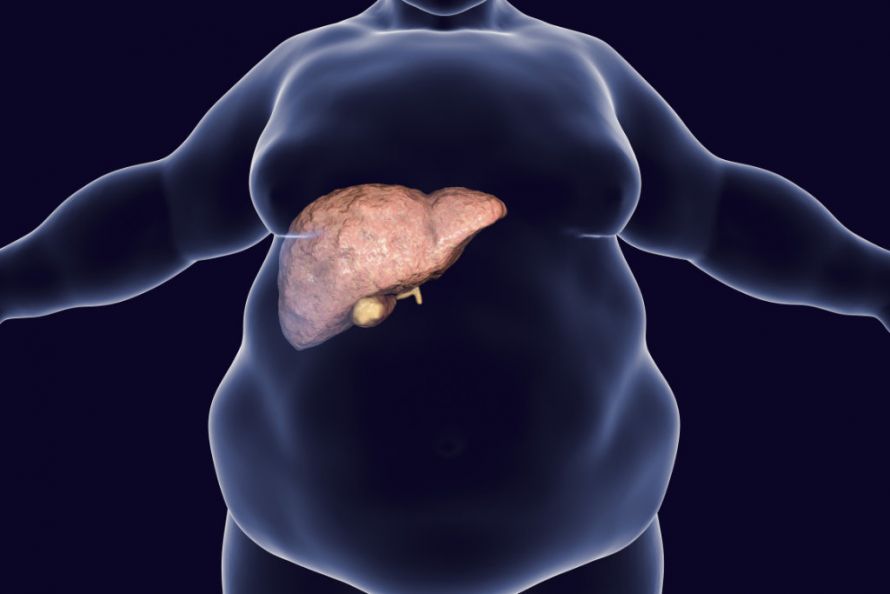
Fatty liver disease is often caused by being overweight © Kateryna_Kon | AdobeStock
Frequency of fatty liver disease
Fatty liver disease occurs with great frequency, especially in Western industrialized countries. There, fatty liver disease is one of the most common liver diseases. In Germany, for example, an estimated 20 to 30 percent of the population suffers from non-alcoholic fatty liver disease. In diabetics, the incidence is said to be as high as 50 percent.
Overall, fatty liver disease is responsible for about 10 to 20 percent of cases of liver cirrhosis and hepatocellular carcinomas (liver cancer).
Causes of fatty liver disease
The cause of fatty liver disease in Western industrialized countries is, in most cases, too frequent and excessive alcohol consumption and metabolic syndrome. The latter is a combination of obesity, type 2 diabetes mellitus, and elevated blood lipid levels.
The amount of alcohol an individual can consume before developing alcoholic liver disease varies from individual to individual. The critical upper limit is considered to be a daily consumption of 10 grams of alcohol for women and 20 grams of alcohol for men. This is equivalent to one-eighth or one-quarter liter of wine or one or two glasses of beer (0.3 liter).
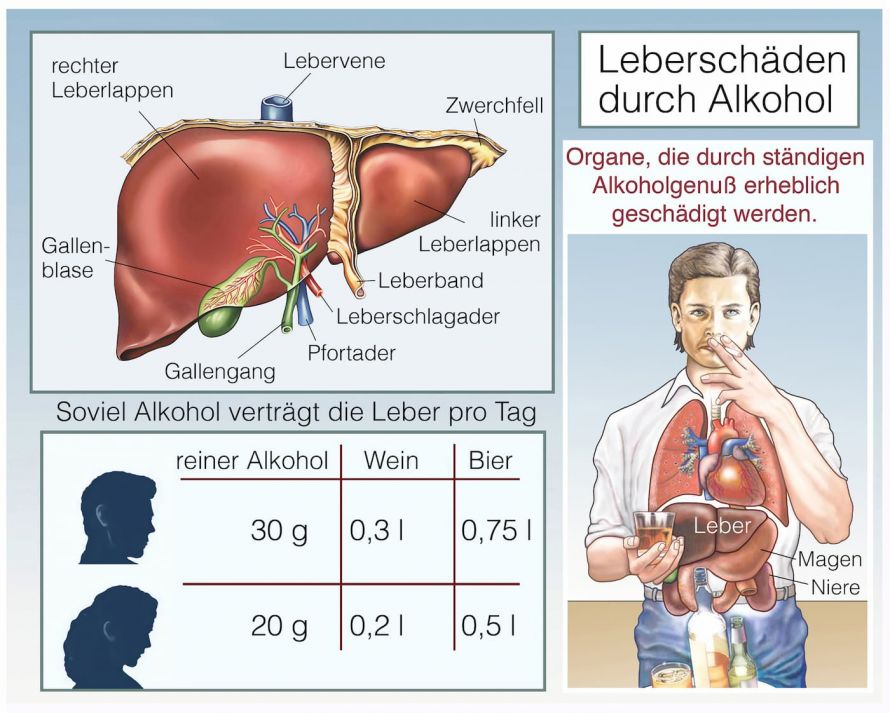
Alcohol is a major cause of liver damage such as fatty liver disease © Henrie | AdobeStock
Other possible causes of fatty liver disease include other diseases such as
- Dyslipidemia,
- Celiac disease (gluten intolerance),
- Chronic viral hepatitis,
- HIV infection,
- Iron and copper accumulation diseases, or
- Gaucher's disease.
Other possible risk factors for the development of fatty liver disease include
- Long-term use of drugs that damage the liver (e.g., cortisone, aspirin, tetracyclines, amiodarone, methotrexate),
- Unhealthy diet, and
- Stressful situations for the body (such as prolonged starvation or artificial feeding).

An unhealthy diet as a risk factor for the development of fatty liver disease © happy_lark | AdobeStock
Fatty liver disease can also especially occur in the last months of pregnancy. However, this is usually harmless. In contrast, patients with acute fatty liver in pregnancy require clinical management.
In addition to unknown causes, genetic factors (such as variants of the gene product PNPLA3) appear to play a role in some cases. They may be responsible for the development of fatty liver disease and, in particular, for its progression to hepatic fibrosis, cirrhosis, and hepatocellular carcinoma.
Symptoms of fatty liver disease
A liver with only small amounts of fat does not cause any symptoms. As the fatty accumulation increases, the liver becomes larger. Some of the more nonspecific symptoms that can occur with a fatty liver include
- Slight pain or
- A feeling of pressure or fullness in the upper right abdomen,
- Loss of appetite,
- Flatulence, and
- Nausea and vomiting.
Fever and a yellowing of the skin (jaundice) are also possible symptoms of fatty liver disease. However, these symptoms usually only appear when the fatty liver turns into fatty liver inflammation (steatohepatitis).

Jaundice indicates liver damage such as fatty liver disease © Daria | AdobeStock
About 30 percent of patients with fatty liver disease have signs of fatty liver inflammation. This is even the case for 50 percent of obese patients with fatty liver disease.
Complications of fatty liver disease can include damage to the cardiovascular system, which can be manifested as atherosclerosis, hypertension, and circulatory disorders, etc. These in turn can lead to serious diseases.
Diagnosing fatty liver disease
The disease is usually diagnosed based on
- The medical history of the person concerned (anamnesis),
- A physical exam,
- A blood test, and
- An ultrasound examination of the abdomen.
When discussing the medical history, the doctor first asks the patient questions about
- The symptoms,
- Existing conditions,
- Eating habits, and
- The consumption of alcohol.
During the physical exam, the doctor palpates the abdomen to determine if the liver is abnormally enlarged.

Palpation examination of the upper right abdomen © pressmaster | AdobeStock
The following values are determined as part of the laboratory diagnostic blood test:
- Liver function test (gamma-GT, AST, ALT, alkaline phosphatase),
- Blood lipid levels (triglycerides, cholesterol, HDL cholesterol, LDL cholesterol), and
- Other blood values (such as bilirubin, fasting blood glucose, or HbA1c).
However, laboratory values alone do not provide evidence of fatty liver disease. This is because the liver values are not necessarily elevated in patients with a fatty liver, for example. However, certain molecular markers (e.g., M30, M65, adiponectin) may also indicate liver injury.
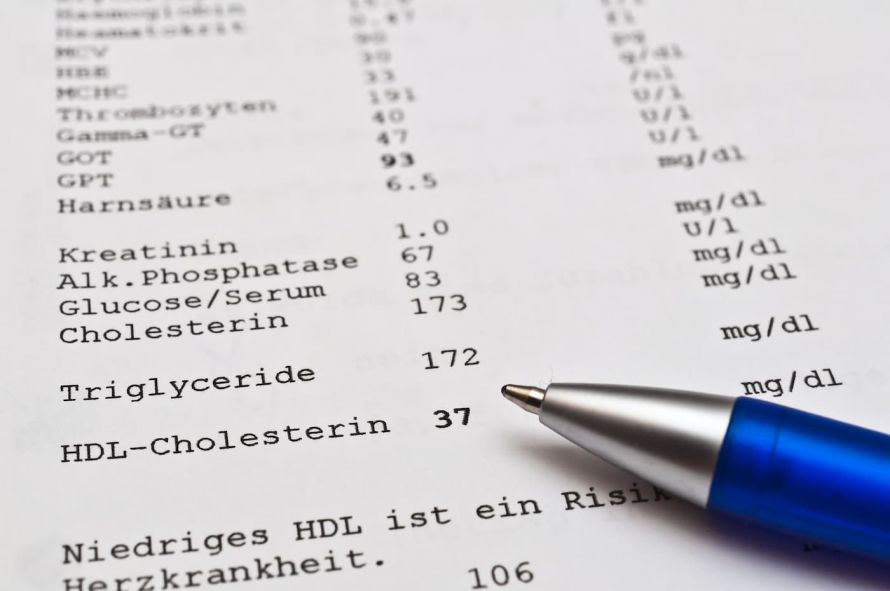
Evaluation of a laboratory diagnostic blood test © Stockfotos-MG | AdobeStock
An ultrasound examination of the abdomen shows the changes typical of a fatty liver. In some cases, a magnetic resonance imaging can provide further helpful information.
If there is a suspicion that hepatic fibrosis or cirrhosis has already developed, the physician may perform an elastography. This is a diagnostic procedure that can determine the stiffness and possibly the fat content of the liver.
To confirm the diagnosis of fatty liver disease and determine the causes and extent of fatty liver, it is necessary to perform a puncture of the liver (liver biopsy). In this procedure, the physician removes a small tissue sample from the liver under local anesthesia using a special hollow needle. He then has these microscopically examined in the laboratory.
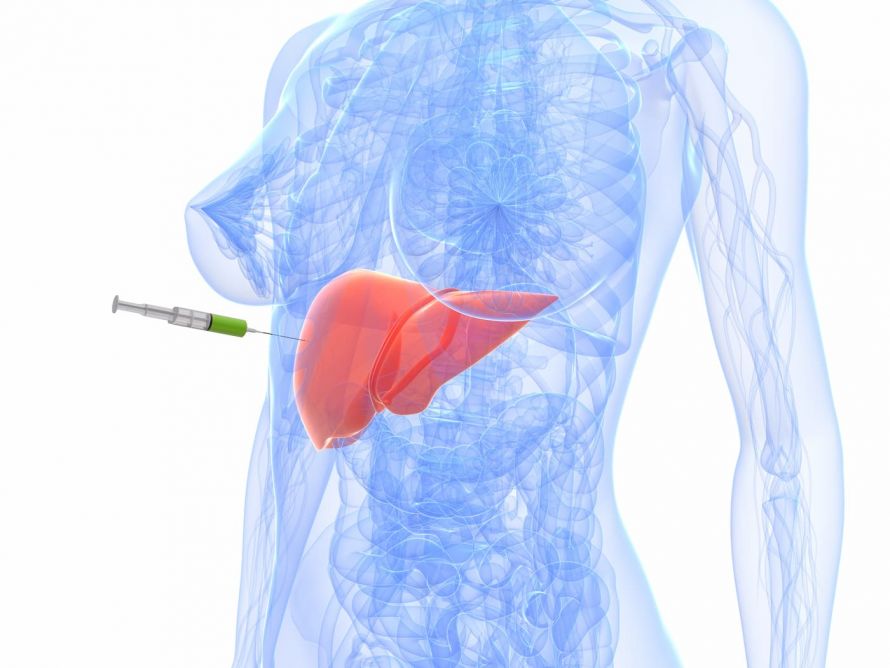
Liver biopsy © SciePro | AdobeStock
Today, a so-called PNPLA3 gene marker can be used to assess the risk of fatty liver developing into hepatic fibrosis, liver cirrhosis, and hepatocellular carcinoma as the disease progresses.
Treating fatty liver disease
Specific treatment of a fatty liver itself, for example with medication, is currently not yet possible.
Rather, the therapy for fatty liver disease is aimed at counteracting the progression of the disease or reversing it. For this purpose, it is necessary to
- Eliminate or reduce the causes of fat storage in the liver,
- Change one’s lifestyle, and
- Treat the underlying condition.
Depending on the cause of the fatty liver disease, this usually means that sufferers have to give up alcohol and, if they are overweight, change their diet and lose weight. A balanced, low-fat, and low-sugar diet with plenty of proteins and sufficient exercise is important.

Alcoholic liver disease can regress with abstinence from alcohol © Pormezz | AdobeStock
Diabetics should also make sure that their blood glucose levels are well controlled. Those affected should also have any existing dyslipidemia treated, if necessary, by taking lipid or cholesterol-lowering drugs.
In patients, who are massively overweight and for whom conservative weight-loss measures have not been successful, bariatric surgery may be required. For this purpose, patients can choose from among surgical procedures for weight loss surgery such as a gastric bypass or a gastric band.
Patients with liver cirrhosis should undergo ultrasound examination at least every 6 months. During this procedure, the physician examines the liver for developing hepatocellular carcinoma.
Prognosis for fatty liver disease
The prognosis is usually good for fatty liver disease. Most fatty liver diseases can usually be reversed and cured. The prerequisite is the fastest possible elimination of the causes and adequate treatment of the underlying conditions.
In principle, a fatty liver can regress within about 2 to 3 months, provided the affected person abstains from alcohol and eats a balanced, low-fat diet.
However, without countermeasures, a fatty liver can turn into fatty liver inflammation and under certain circumstances, this can develop into cirrhosis of the liver and then hepatocellular carcinoma. These diseases cannot be reversed. A complete cure is then no longer possible.