Here you will find further information and selected spina bifida specialists and centres.
Here you will find further information and selected spina bifida specialists and centres.
Recommended specialists
Brief overview:
- What is spina bifida? A congenital malformation in which the vertebral arches of the spinal column do not close completely, creating a gap in the spine.
- Types: There are two forms: Spina bifida occulta (the spinal cord is not affected) and spina bifida aperta (the spinal cord can protrude from the spinal canal). The first variant occurs more frequently.
- Symptoms: The symptoms can be very different. They depend on whether the spinal cord is affected. The occulta variant often does not cause any symptoms. Otherwise, muscle paralysis, sensory disturbances, disturbed bladder function and others may occur.
- Causes: The cause has not been clarified to date. However, genetic predisposition, folic acid deficiency and various medications taken by the mother during pregnancy seem to increase the risk of the malformation.
- Diagnosis: Often, the disease is detected before birth through amniocentesis, ultrasound scans or a blood test of the mother.
- Treatment: The treatment depends on the severity of the malformation. Mild spina bifida often does not require treatment. Otherwise, the spinal canal is closed shortly after birth. Nevertheless, lifelong care for the affected person is then necessary.
Article overview
What is spina bifida?
In the third to sixth week of pregnancy, the embryo's spinal column and the spinal cord. They arise from the neural tube, an embryonic tissue structure. This is why spina bifida belongs to the so-called neural tube defects.
Normally, the two vertebral arches merge with the vertebral body to form a ring. This ring limits the vortex hole to the back. The spinal cord, which is surrounded by spinal meninges, is located in the vertebral foramen.
In the case of spina bifida, the vertebral arches do not close, creating a vertebral fissure. These occlusion disorders most often affect the lower part of the spine, i.e. the lumbar spine and the sacrum.
Spina bifida is the second most common congenital malformation. However, it only occurs in about one in a thousand children in Central Europe. Girls are affected slightly more often than boys.
What are the different forms of spina bifida?
In medicine, a distinction is made between two forms:
- Spina bifida occulta (Latin: occulta = hidden) and
- Spina bifida aperta (Latin: aperta = open, visible), also known as myelocele, myelomeningocele.
the more common spina bifida occulta, in which only the vertebral arch is split without the spinal cord being affected. Thus, the malformation is not visible from the outside and is often only detected by accidental X-ray examinations.
Spina bifida occulta does not usually need to be treated and rarely causes symptoms.
In spina bifida aperta, not only the vertebral arches but also the spinal cord and/or the spinal meninges are split. In this case, the spinal cord is often protruded beyond the spinal canal like a sack. The spinal cord can be covered with a thin skin, but it can also be completely exposed.
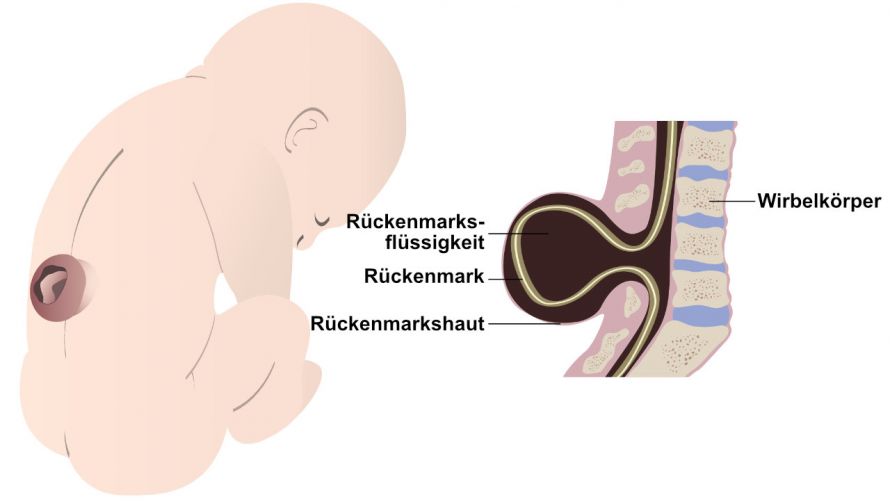
In spina bifida, parts of the spinal cord can bulge outwards © Nattapon | AdobeStock
What are the symptoms or sequelae of spina bifida?
The symptoms and consequential damage in early childhood and in adulthood can be very different. They depend on where the vertebral fissure occurs and whether the spinal cord is affected.
Spina bifida occulta often causes no symptoms at all, as the spinal cord is not affected by the cleft formation.
The situation is different with spina bifida aperta. Here too, however, there are great differences in the intensity of the complaints.
Only slight impairments in walking may occur. Typical follow-on effects are
- Paralysis of the muscles,
- Leg weakness,
- Sensory disturbances,
- Curvatures and malpositions of the joints as well as
- Impairment of the gastrointestinal system.
Often there is a disturbed bladder function. Infections of the urethra and discharge problems (e.g. incontinence) are typical consequences. In the worst case, paraplegia can occur.
A phenomenon that often occurs together with spina bifida is so-called hydrocephalus. Cerebrospinal fluid accumulates owing to the disturbed circulation. Hydrocephalus can lead to impaired performance and epileptic seizures.
What are the causes of spina bifida?
The cause of the neural tube defect is still unknown. Genetic factors probably play an important role. If one child has already been born with spina bifida, the risk for the second child increases by about 40 percent.
External influences also seem to promote spina bifida. A deficiency of folic acid is considered a significant risk factor. Doctors recommend that women with folic acid deficiency take folic acid supplements even before they plan to become pregnant.
Furthermore
- Medication for epilepsy,
- Gestational diabetes and the
- Mother being overweight
also contribute to a malformation. Women with epilepsy should discuss alternative treatment with their doctor.
How is spina bifida diagnosed?
Suspicion of spina bifida can be ruled out before birth by an amniocentesis test. However, this investigation does not provide one hundred percent certainty.
Ultrasound examinations from the 12th week of pregnancy are usually more reliable. They can make spina bifida recognisable at an early stage. A blood test of the mother in the 16th week of pregnancy can enable a diagnosis to be made.
After birth, severe spina bifida is visible to doctors with the naked eye. The newborn's back is strongly arched in this case.
The actual extent of the malformation is determined with the help of various procedures such as X-ray examinations and computer tomography.
Doctors from many disciplines work together to examine the child holistically. These include paediatric neurologists and paediatric orthopaedists.
How is spina bifida treated?
The treatment of spina bifida depends on the severity of the malformation.
Mild spina bifida often does not require treatment. The treatment of a more severe form is carried out on an interdisciplinary basis by
- Paediatricians,
- Paediatric surgeons,
- Neurosurgeons,
- Neurologists,
- Orthopaedic surgeons,
- Paediatric urologists,
- Speech therapists,
- Physiotherapists and
- Psychologists.
The child should achieve good mobility in order to be able to participate almost fully in everyday life. An open spine is surgically closed by doctors shortly after birth to prevent germs from entering the spinal cord.
If hydrocephalus is present, a catheter is placed to allow the cerebrospinal fluid to drain. For disorders of the bladder a catheter can also be placed. Walking and standing can be made easier with various orthopaedic aids. Operations can also correct certain malpositions.
The treatment of severe spina bifida includes lifelong and multidisciplinary care for the affected person.
Further information on spina bifida can be found on the website of the Federal Association for the Support of Families of Prenatally Ill Children e.V.













