Women and men are affected by anal fissures at about the same frequency. Most patients are between 40 and 50 years old at diagnosis, but children can also develop anal fissures.
Most anal fissures heal spontaneously. In the case of anal fissures that do not heal, medications or surgery usually help, so healing is possible even in these cases.
Depending on how long the mucosal tear has been present, it is referred to as
- An acute anal fissure, or
- A chronic anal fissure.
If the tear has been present for less than six weeks, the patient is suffering from an acute anal fissure. If it lasts more than six to eight weeks, the patient has a chronic anal fissure.
Furthermore, depending on the cause, a distinction is made between primary and secondary anal fissures. In the case of secondary instances, the fissure is caused by another disease. This is not the case with primary anal fissures.
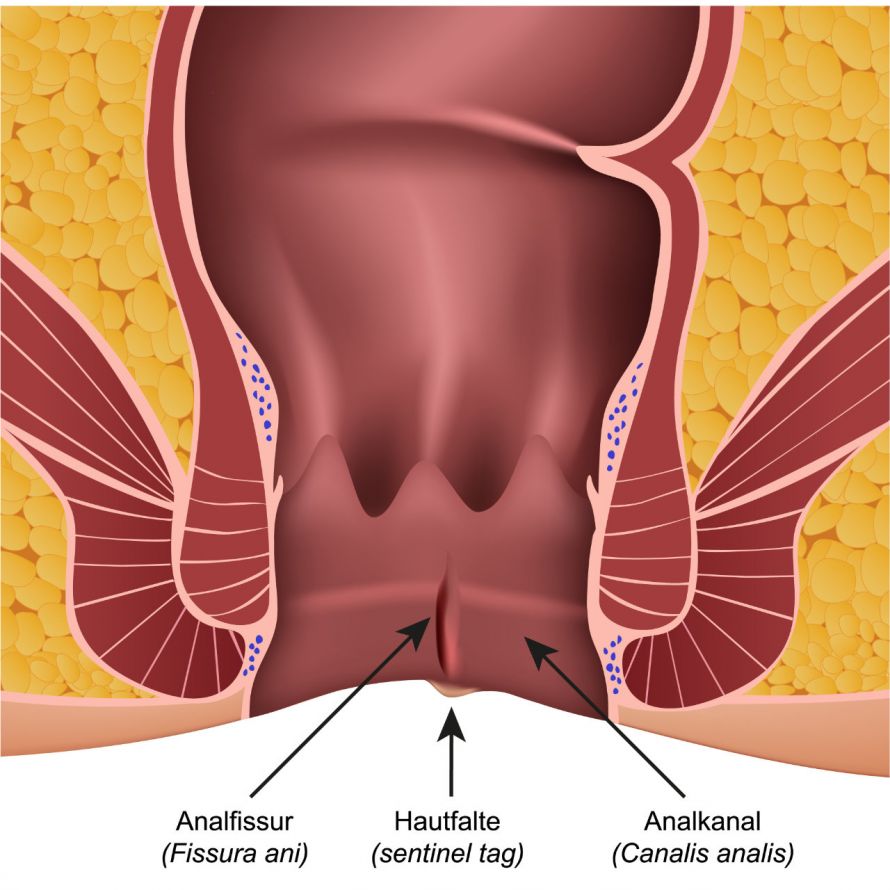
Rhagades must be distinguished from anal fissures. These are skin tears around the anus, not mucous membrane tearing of the anal canal.
Most anal fissures are located on the lowest section of the anal opening facing the back and may be visible from the outside. However, it can also be located on the inside and then only found on closer inspection of the anal canal.
During bowel movements, some patients experience pain. They usually last for a few minutes but can also last for hours. Some bright red blood can often be found on toilet paper and sometimes on the stool. Without a bowel movement, however, most patients have no complaints.
Occasionally, itching and a rash will occur around the anus.
In the case of chronic anal fissures, secondary conditions may develop around the tear in the mucosa such as enlarged anal papillae. These are nodules about the size of a pinhead in the mucosa. In the case of anal fissures, they can grow to the size of a cherry. Then they are also called anal polyps or anal fibromas.
Additionally, sentinel piles can occur. Sentinel piles are skin tags around the anus and are therefore also called anal tags or rectal skin tags.
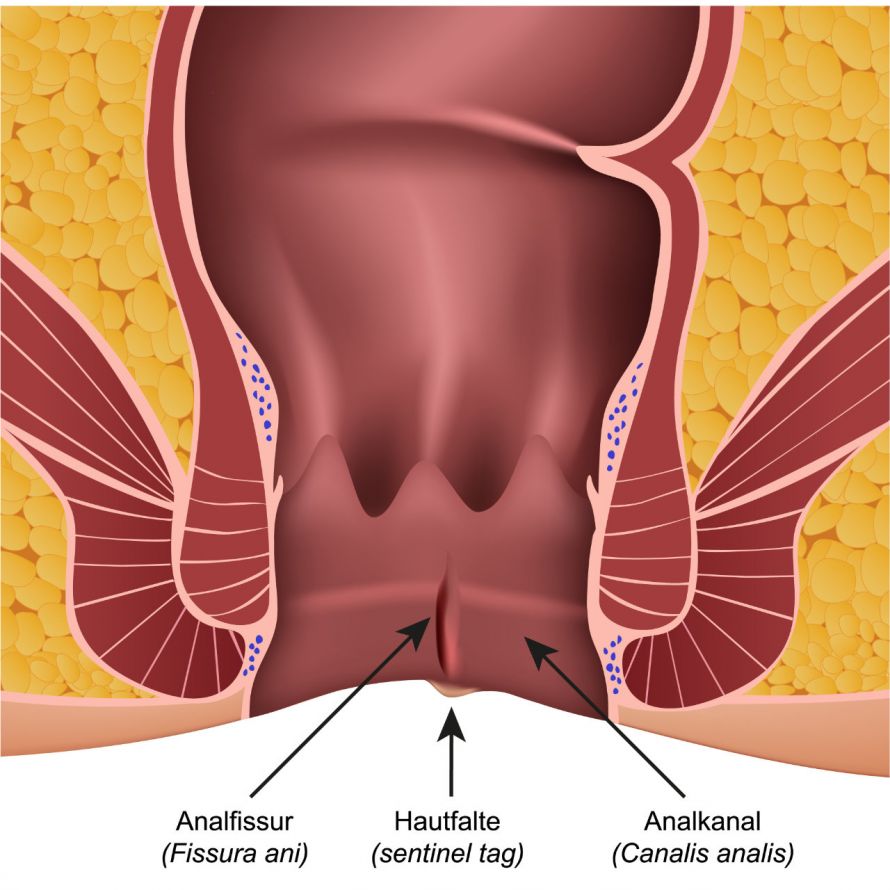
An anal fissure is a small wound in the mucosa of the anal canal © bilderzwerg | AdobeStock
In most cases, the cause of anal fissure cannot be identified. In such cases, doctors use the term primary anal fissure.
While it has not yet been precisely understood how primary anal fissures develop, it is suspected that
play a role in their formation.
As a result of the pain caused by the tear, the sphincter muscle contracts spasmodically. The sphincter surrounds the anal canal and regulates defecation. The increase in sphincter pressure worsens the supply of blood to the mucous membrane. This in turn has a negative effect on the wound healing process.
Thus, an acute anal fissure can develop into a chronic condition.
Secondary anal fissures are tears that occur due to another condition or injury. Their triggers may include:
Conditions that increase the likelihood of developing constipation and hard stools, thus increasing pressure in the sphincter muscle, are considered risk factors. These include for example
Other risk factors include the insertion of foreign objects into the anal canal and rough anal intercourse.
First and foremost, the doctor examines the anus and anal canal. Often the examiner can already see the anal fissure by spreading the buttocks. It is also usually possible to distinguish at this stage whether an anal fissure or a hemorrhoid is present.
As a rule, the proctologist then palpates the anal canal with a finger (digital-rectal examination). Besides being usually painful in cases of acute anal fissures, the examination is also not always necessary. Chronic anal fissures are less painful. Here, the physician can use digital-rectal examination to detect cicatricial hardening, where appropriate.
Using an anal spreader or a proctoscope (a short tube with a light source), the doctor assesses the anal canal. This proctoscopy is also known as
- An anal endoscopy,
- A rectoscopy, or
- An endoscopy of the rectum
This examination provides further information about changes in the anal canal, which show similar symptoms to anal fissures and must therefore be excluded.
Because of the pain that may be expected during the proctoscopy, the physician may also attempt treatment first. The prerequisite for this is a typical pathology and a visible mucosal tear.
However, if there is any doubt about the diagnosis, an anal endoscopy must be performed. Then one is performed under local anesthesia or general anesthesia.
Further examinations are only considered in rare cases. They include
They are used to exclude other diseases or to diagnose underlying diseases.
Proctologists are specialists in anal fissures and they treat diseases of the rectum and anal canal.
Treatment is aimed at regulating the stool through diet. It also addresses pain, especially in acute anal fissures, and attempts to decrease sphincter pressure.
Diet
An important component of treatment is a high-fiber diet. In addition, psyllium husks, for instance, can help regulate bowel movements.
However, the stool may not become liquid. Therefore, you should not take strong laxatives as treatment.
Drug therapy: Creams, ointments, tampons, and syringes
Local application of ointments or creams usually helps considerably. As a result, most acute anal fissures heal within six to eight weeks. In studies, calcium channel blockers (for example, nifedipine and diltiazem) have been shown to be particularly effective.
Just like nitrates (for example glyceryl trinitrate), these medicines lower the pressure in the sphincter muscle or relax it. However, nitrates often cause headaches.
If eczema is present in addition to an anal fissure, the use of creams or ointments containing cortisone is also recommended. Topical ointments with local anesthetics (lidocaine) can be used to treat acute pain.
Some medications are inserted into the anal canal with the help of anal tampons, thereby releasing the active ingredients over a longer period of time.
Anal dilators
Anal dilators (rectal dilators), which are inserted into the anal canal, can also support healing. They are used on their own or in combination with the above-mentioned drugs.
You can perform anal stretching independently and carefully several times a day.
Do home remedies, sitz baths, etc., help against anal fissures?
Home remedies such as sitz baths and natural remedies may be pleasant, but they do not heal anal fissures. You should not use zinc ointments on open wounds such as an anal fissure.
Bepanthen is said to promote the healing of small lacerations. However, current guidelines do not mention it as a treatment option.
If healing does not occur after six to eight weeks of medication-based treatment, then surgery becomes a possible option. It is often used to treat chronic anal fissures. The following surgical procedures have become established:
Fissurectomy (= cutting out the anal fissure): According to guidelines, it is the therapy of choice. Together with the inflamed and scarred tissue, the fissure is cut out. The wound is not sutured and the sphincter muscle remains intact. Sometimes a mucosal or skin flap is placed over the excised area and sutured (anal advancement flap). Fissurectomies have a higher rate of success than drug therapy approaches.
Fissurectomy with a co-administration of botulinum toxin: The sphincter muscle is additionally relaxed with the help of "Botox". This could be more advantageous than solely excising the fissure.
Separating the sphincter muscle (sphincterotomy): Severing part of the internal sphincter has a higher success rate than fissurectomies. However, it does increase the risk of developing fecal incontinence after the procedure.
There are other, additional procedures, but they have not yet become established. This includes, for instance, treatment with a fractional CO2 laser.
Generally, the surgery is performed on an outpatient basis and the patient undergoes short-term anesthesia. After the surgery, there is usually pain in the anal region for a few days. However, this pain quickly improves.
The resulting open wound will need to be kept clean for several weeks until it heals completely. To do this, you should wash the wound several times a day and after each bowel movement. Sitz baths are not necessary. On the contrary: They tend to slow down healing.
Many acute anal fissures regress spontaneously, i.e., without treatment. With the help of medication and physical therapy, up to 90 percent of acute anal fissures heal. In the chronic form, the rate of healing for this treatment is still about 50 percent.
However, the chances of recovery are very good with the help of surgical treatment options. The cure rates are about 73 to 80 percent for fissurectomies and about 80 to 93 percent for sphincterotomies.
It should be noted, however, that this poses an increased risk of fecal incontinence. After a fissurectomy, up to about eleven percent of patients suffer from this. After a sphincterotomy, this number rises up to even 20 percent.
Some patients develop an anal fissure again after a few years (so-called recurrence). To prevent anal fissures and their recurrence, it is necessary to adopt an appropriate diet.
A diet rich in fiber and roughage, possibly supported by psyllium husks, will help you regulate the consistency of your stool. Anal dilators can also be used to prevent recurrence.