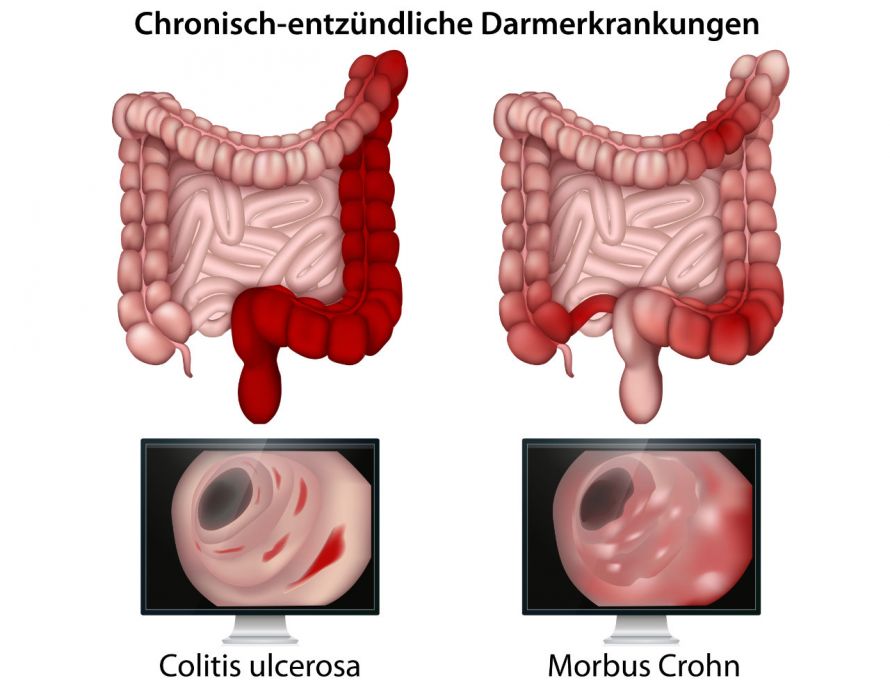
Crohn's disease like ulcerative colitis is a chronic inflammation of the gastrointestinal tract. It is also known as enteritis regionalis Crohn, enteritis terminalis, ileitis terminalis or scarring enteritis. The disease usually progresses in episodes and is not contagious.
The entire gastrointestinal tract, i.e. from the mouth to the anus, can be affected by Crohn's disease. However, the disease usually manifests itself in the area of the lowest section of the small intestine, at the transition to the large intestine.
Here
- Fistulas,
- Constrictions and
- Ulcers develop in all layers of the intestinal wall.
In contrast, ulcerative colitis only occurs in the large intestine and affects the intestinal mucosa exclusively superficially. In Crohn's disease, deeper layers of the intestinal wall can also be affected by the inflammation.
Depending on the affected section, a distinction is made, for example:
- Crohn's disease with ileocecal involvement: Here, the small intestine incision and appendix (cecum) are inflamed
- Crohn's colitis: all or part of the colon is inflamed
Crohn's disease in numbers
Crohn's disease is one of the most common chronic inflammatory bowel diseases:
- Out of every 100,000 inhabitants, about 120 to 200 suffer from Crohn's disease.
- Every year, between 5.2 and 8.6 people per 100,000 inhabitants in Central Europe are newly diagnosed with Crohn's disease.
- In Germany, about 5 people per 100,000 inhabitants contract Crohn's disease every year.
- In principle, the disease can occur at any age. However, young adults between the ages of 15 and 35 are most often affected by Crohn's disease. In about 15 to 25 percent of all those affected, the first symptoms appear before the age of 20. Some symptoms may even start in infancy.
- The activity of the disease often decreases in older age.
- Crohn's disease occurs about equally often in women and men.
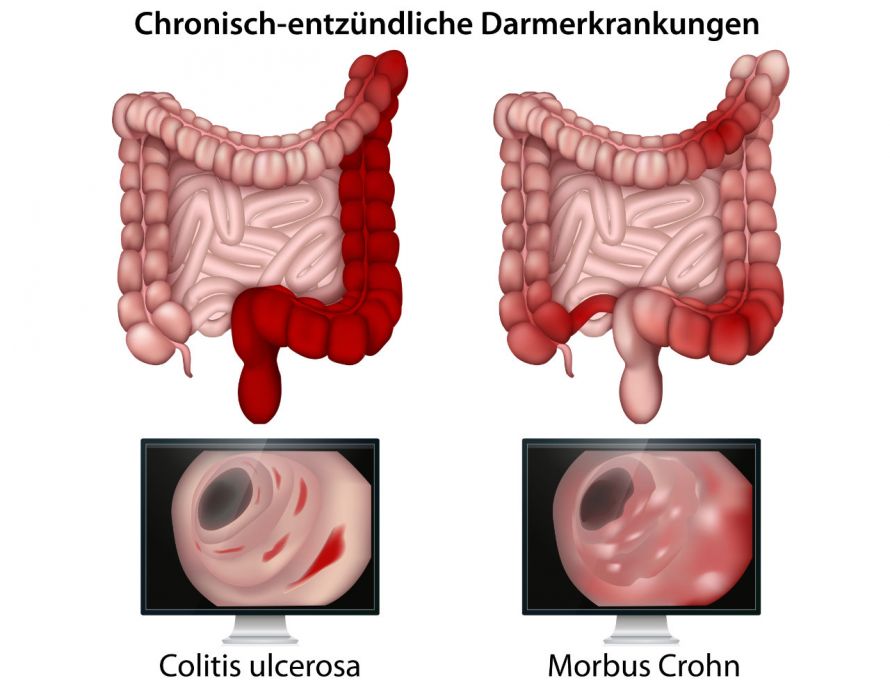
Comparison of the effects of ulcerative colitis and Crohn's disease © bilderzwerg | AdobeStock
The causes for the development of Crohn's disease are not precisely known. However, due to the familial accumulation of the disease, it is assumed that there is a hereditary predisposition. If a close relative already has Crohn's disease, then there is about a tenfold increased risk for the other family members.
In addition, disorders of the immune system are discussed, which lead to pathological interactions with the intestinal wall and thus to the inflammations.
Environmental factors seem to play a role in the development of Crohn's disease as further causes. For example, smokers and people from industrialised nations have a higher risk.
Psychological factors (e.g. psychological strain, stress) do not influence the development, but they do influence the progression of the disease. Diet, on the other hand, is not responsible for either the onset or the episodes.
Crohn's disease is typically characterised by
- cramping abdominal pain mostly in the right lower abdomen and
- watery, sometimes also mucous diarrhoea which lasts for several weeks and rarely contains blood.
This is usually accompanied by a lack of appetite and weight loss. The symptoms are similar to those of ulcerative colitis.
The exact symptoms depend, among other things, on which section of the digestive system is affected by the inflammation. Some sufferers experience only mild symptoms, while others suffer severe discomfort.
In addition, the symptoms can be non-specific, especially at the beginning of the disease. In children, Crohn's disease can also be manifested by slower growth and a later onset of sexual maturity.
Since inflammation can also occur outside the intestine, so-called extraintestinal manifestations can also occur. These include:
- Pain in the knee or ankle joint
- inflammatory skin changes
- chronic fatigue (fatigue syndrome)
Crohn's disease has a chronic and spasmodic progression in which the disease activity increases and then decreases. Depending on the severity of the inflammation, an acute Crohn's disease flare-up is therefore classified as mild, moderate or high.
Crohn's disease can affect only a single section or several areas of the digestive tract at the same time. The following sections are most frequently affected:
- Lower section of the small intestine (terminal ileum): about 30 per cent of cases
- Transition from the small intestine to the large intestine (ileocolon): about 40 per cent of cases
- Large intestine and anal canal: about 25 per cent of cases
- Other sections: about 5 per cent of cases
Although Crohn's disease is a long-lasting illness, the life expectancy of patients is hardly affected. The majority of patients can lead a largely normal life.
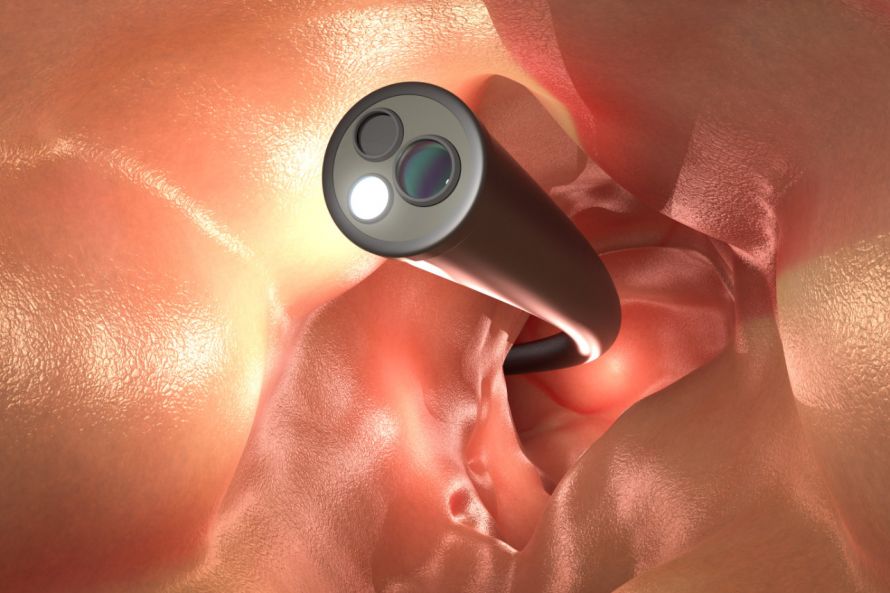
The following video shows the findings in the colonoscopy:
Depending on the extent and duration of the disease, complications may occur. However, this is rather rarely the case. The occurrence of a complication can often be an indication for Crohn's disease surgery.
The most important complications of Crohn's disease occur in the area of the intestine occur:
- Narrowing (stenoses)
- Intestinal obstruction: Depending on the cause, Crohn's disease surgery may be necessary
- Intestinal perforation: life-threatening complication requiring immediate Crohn's disease surgery
- Fistulas (connecting ducts mostly between bowel segments or between bowel and skin)
- Fissures (tears, mostly at the anus and in the anal canal)
- Abscesses (accumulation of pus, especially in the anal area)
- Conglomerate tumour (inflamed intestinal loops stuck together)
- Malabsorption syndrome (lack of nutrients)
- Intestinal bleeding: If it is no longer possible to compensate for the blood loss with blood transfusions, Crohn's disease surgery is necessary.
The main complications of Crohn's disease outside the bowel are:
At the beginning of the diagnosis, the patient is usually asked in detail (anamnesis) about
- Symptoms
- Medical history
- Family history
This is followed by physical and other examinations.
During the physical examination, the abdominal cavity is palpated. The doctor looks for pressure pain in the right lower abdomen and for hardening. The anus is examined for fistulas and fissures.
Blood test: Certain changes can be detected in the blood count. Often
- anaemia is present.
- the erythrocyte sedimentation rate (ESR) and the leucocyte count are often elevated,
- an elevated CRP value indicates an acute inflammatory process and
- folic acid, vitamin D and vitamin B12 may be reduced.

Some blood tests can indicate Crohn's disease © Henrik Dolle | AdobeStock
A colonoscopy allows, in addition to the visual assessment of the intestine, the removal of tissue samples from the mucous membrane in order to confirm the diagnosis on a histological basis.
An ultrasound examination (sonography) can be used to check whether the bowel wall is thickened.
Furthermore gastroscopy and other imaging procedures such as magnetic resonance imaging (MRT) may be necessary.
Since it is unknown why Crohn's disease develops, the disease cannot be cured. Therefore, the treatment of Crohn's disease primarily pursues the goal,
- of stopping the inflammatory process,
- alleviating the discomfort and
- reducing the risk of complications.
Depending on the severity and progression, different options are available for the treatment of Crohn's disease:
- During an acute episode of the disease, drug treatment (e.g. cortisone or special anti-inflammatory drugs) is administered. In the case of repeated episodes, permanent medication may also be necessary.
- Dietary changes in children and in underweight patients or intake of important nutrients if there is a nutrient deficiency may be necessary.
- In the case of complications such as fistulas or intestinal obstruction, or if drug treatment does not respond, surgical treatment (Crohn's disease surgery) is necessary.
Surgical treatment of Crohn's disease
Crohn's disease surgery is an important treatment option for patients with Crohn's disease, as the following figures show:
- In 80 percent of Crohn's disease patients, the first Crohn's disease operation is performed about 10 years after the onset of the disease.
- About 90 percent of Crohn's disease patients have to undergo Crohn's disease surgery at least once in their lives.
The most important reasons for Crohn's disease surgery are
- intestinal obstruction (ileus),
- a rupture of the intestine (perforation) or
- severe bleeding.
Crohn's disease surgery at the right time can prevent discomfort and complications.
During surgery, the minimum amount of small intestine is removed, because despite resection (removal), recurrence can occur.
The aim of Crohn's disease surgery
Two types of Crohn's disease surgery can be distinguished:
- Emergency Crohn's disease surgery is required for conditions that may be life-threatening. These include, for example, stenosis (narrowing of the bowel) and intestinal obstruction (ileus), peritonitis (inflammation of the peritoneum) and perforation of the bowel.
- Elective Crohn's disease operations are part of an individual treatment concept and can be planned in the long term. Elective Crohn's disease surgery accounts for the vast majority of all Crohn's disease operations.
Indications for Crohn's disease surgery
Surgery cannot cure the disease. Even after a Crohn's disease operation, there is a risk of relapse (recurrence). Therefore, the pros and cons of an operation for Crohn's disease must be clarified individually.
In principle, however, the following indications exist for Crohn's disease surgery:
- Therapy-refractory Crohn's disease (drug treatment does not respond sufficiently): elective indication
- Incomplete/chronic bowel obstruction that cannot be treated: elective indication
- Complete intestinal obstruction: emergency indication
- Diagnosed precancerous lesions (low-grade intraepithelial neoplasia): elective indication
- Toxic megacolon (dilatation of the colon with harmful accumulation of intestinal contents): urgent indication
- Perforation (intestinal rupture): emergency indication
- Severe intestinal bleeding: urgent indication
- Peritonitis (inflammation of the peritoneum): emergency indication
In the following cases, Crohn's disease surgery should be postponed as long as possible:
- In the presence of abscesses
- In the presence of fistulae
- In the presence of conglomerate tumours
Diagnostics before surgery for Crohn's disease
If a Crohn's disease operation is planned, the following are carried out in advance in particular
- a colonoscopy,
- sonographic and radiological assessment of the small intestine and
- the determination of some laboratory values.
The diagnosis before surgery for Crohn's disease should answer the following questions:
- Is it really Crohn's disease (or perhaps ulcerative colitis or another chronic inflammatory bowel disease)?
- What is the disease pattern or how has the disease spread?
- Is there a typical indication for Crohn's disease surgery?
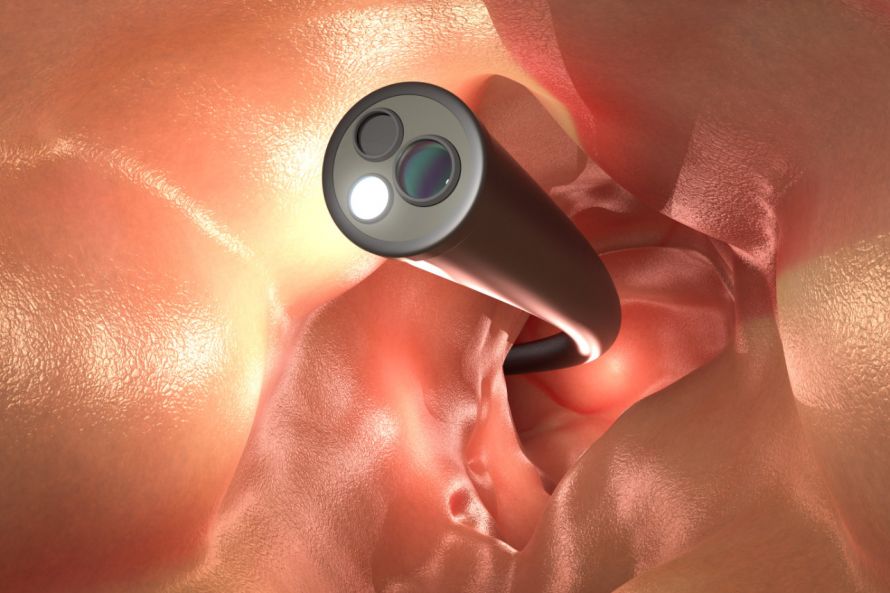
A colonoscopy is one of the important diagnostic examinations prior to Crohn's disease surgery © phonlamaiphoto | AdobeStock
Procedure for Crohn's disease surgery
The most common procedures for Crohn's disease surgery are
- bowel resection (removal of parts of the bowel),
- Removal of fistulas and
- Drainage of abscesses.
Crohn's disease surgery is only performed on the affected section of the bowel. Radical Crohn's disease surgery, i.e. removal of large sections of bowel, has been shown to be disadvantageous and is therefore avoided. Surgery is only performed on an inflamed area when it causes discomfort.
Occasionally, scars or adhesions can cause narrowing (stenosis) in the bowel. This prevents the transport of the intestinal contents. Then removal of the affected section of bowel becomes necessary.
Crohn's disease surgery for stenosis consists of sparingly removing the narrowed segment of bowel. In the case of short stenoses (strictures), plastic dilatation is sometimes sufficient without having to remove the intestinal tissue itself. By restoring unrestricted stool passage (stricturoplasty), the inflammation heals and the patient becomes symptom-free.
Fistulas from the intestine to the bladder (enterovesical fistulas) and fistulas ending blindly in the posterior abdominal cavity can be dangerous. They can affect other organs (e.g. the urogenital tract) or lead to dangerous accumulations of pus in the body (abscesses). After removal of the diseased bowel sections, the fistula usually heals quickly.
An abscess can either be punctured or the fluid drained via a drainage tube.
Emergency surgery for Crohn's disease
Fortunately, real emergencies are rare in Crohn's surgery. The figures are slightly below 5 per cent of all surgical procedures.
Emergency indications are
- intestinal perforation (as a result of severe inflammation or also after colonoscopies),
- severe intestinal bleeding,
- acute most severe inflammation and
- sudden total intestinal obstruction (ileus).
In all these situations, action must always be taken immediately and the results are somewhat worse than in planned Crohn's disease operations. However, emergency operations should be the exception in good medical care for Crohn's patients!
For Crohn's disease surgery, a specialist in visceral surgery or a specialist in general surgery is responsible.