Recommended specialists
Brief overview:
- What is ulcerative colitis? A chronic, inflammatory condition of the mucous membrane of the large intestine that mainly affects young adults between the ages of 15 and 30.
- Causes: Since the disease runs in families, it is assumed to be hereditary. Other risk factors: Immune system disorders as well as psychosomatic factors, nutrition, viruses and bacteria.
- Symptoms: Cramping abdominal pain, also before or after bowel movements, bloody and mucous diarrhoea, lassitude, loss of appetite, nausea, Anaemia and others.
- Types: Chronic-recurrent (most common form, relapsing course, lasts for years), chronic-continuous (constant complaints, no phases), acute-fulminant (very sudden, violent onset of disease).
- Complications: The disease can cause serious complications, including: Intestinal rupture, severe intestinal bleeding, scarring, fistulas and abscesses, inflammation of the bile ducts, liver damage and others.
- Diagnosis: The anamnesis and physical examinations are often followed by a colonoscopy a blood test and a stool test, ultrasound and an X-ray.
- Treatment: Cure is not possible, instead discomfort should be alleviated. In addition, there is the possibility of using medication, a change in diet and SURGERY.
Article overview
What is ulcerative colitis and how does the disease manifest itself?
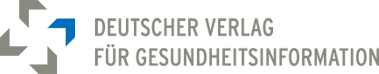
Ulcerative colitis and Crohn's disease are chronic inflammations of the intestinal mucosa of the large intestine that usually occur in episodes. Both diseases belong to the group of chronic inflammatory bowel diseases.
While Crohn's disease usually occurs in the small intestine, but can also occur in the entire gastrointestinal tract, ulcerative colitis only occurs in the large intestine.
The inflammation of the bowel usually begins in the rectum. It then often extends first to the left side, but possibly also to the entire colon. A transition to the small intestine occurs only very rarely.
Just like Crohn's disease, ulcerative colitis is an inflammatory bowel disease © bilderzwerg | AdobeStock
Ulcerative colitis in numbers
Ulcerative colitis is one of the most common chronic inflammatory bowel diseases:
- Out of every 100,000 inhabitants, about 120 to 200 suffer from ulcerative colitis.
- Every year, between 5 and 10 people per 100,000 inhabitants in Central Europe develop ulcerative colitis.
- In principle, the disease can occur at any age. However, young adults between the ages of 15 and 30 are most commonly affected by ulcerative colitis. In about 25 per cent of all those affected, the first symptoms appear before the age of 20. In some cases, this can even be as early as infancy.
- Ulcerative colitis is slightly more common in women than in men.
Causes of ulcerative colitis
The causes of ulcerative colitis are not known. However, due to the familial accumulation of the disease, it is assumed that there is a hereditary predisposition. Furthermore, disorders of the immune system could lead to pathological interactions with the intestinal mucosa and thus to the inflammations in the colon.
Other causes are
- psychosomatic factors (e.g. psychological strain, stress),
- nutritional factors,
- but also viruses and bacteria.
Diagnosis of ulcerative colitis
The diagnosis of ulcerative colitis usually begins with a questionnaire about existing symptoms and medical history (anamnesis). This is followed by a physical examination.
Further examinations may include:
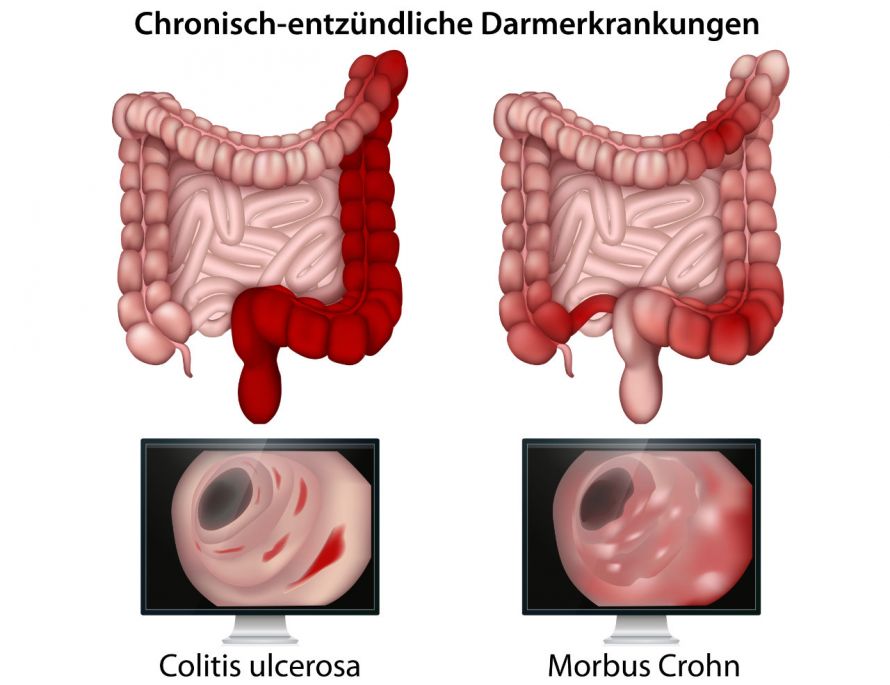
- Colonoscopy for visual assessment of the intestine and for taking tissue samples of the intestinal mucosa
- Blood test with test of the inflammation values to exclude a bacterial infection
- Stool examination to exclude pathogen-induced intestinal inflammation
- Ultrasound (sonography) for an overview of the anatomical situation in the abdominal cavity
- X-ray contrast examination for better assessment of the colon
Before a planned colitis ulcerosa operation, an endoscopy of the rectum (rectoscopy) is necessary.
A colonoscopy allows the doctor to take a close look at the intestines © phonlamaiphoto | AdobeStock
Symptoms of ulcerative colitis
Ulcerative colitis is typically characterised by cramping abdominal pain
- in the left lower abdomen,
- in the middle of the lower abdomen or
- in the sacrum area.
Patients often have pain before or immediately after defecation.
Furthermore, the intestinal disease is characterised by bloody and mucous, sometimes also watery diarrhoea. The number of diarrhoea cases depends directly on how severely the colon is affected by the disease. Diarrhoea can occur up to 20 times a day, and in severe cases even up to 30 times a day.
Depending on the severity, there may be other symptoms of ulcerative colitis:
- Fatigue, physical weakness, tiredness
- Loss of appetite and nausea
- Anaemia
- Fever
- Weight loss
- Increase in white blood cells (leucocytosis)
Progression of ulcerative colitis
The disease usually shows a chronic and relapsing progression, but can also be rather constant. Thus, three forms can be distinguished:
Chronic recurrent ulcerative colitis is the most common form, affecting about 85 percent of patients. The bowel disease progresses in episodes with phases without signs of disease that can last up to several years. However, this can always be followed by recurrences (relapses).
Chronic continuous ulcerative colitis occurs in about 10 percent of patients. Those affected suffer continuously from discomfort and do not have phases without signs of illness.
Acute fulminant ulcerative colitis affects about 5 percent of patients. This form is characterised by a very sudden and violent onset of disease with
- Severe diarrhoea,
- Abdominal pain and
- Fever.
Complications of ulcerative colitis
Depending on the extent and duration of the inflammation, complications may occur. However, most patients are spared complications. The occurrence of a complication often constitutes an indication for ulcerative colitis surgery.
The main complications of ulcerative colitis in the colon are:
- Toxic megacolon: large intestine overstretched due to wall weakness and gas accumulation.
- Intestinal rupture (perforation): A bowel rupture of ulcerative colitis is a life-threatening complication and must be treated immediately by surgery.
- Severe intestinal bleeding: The blood losses can often be compensated for by blood transfusions. Removal of the affected section of bowel as part of surgery for ulcerative colitis is rarely necessary.
- Scarring (strictures): The scars can lead to narrowing of the bowel and intestinal obstruction requiring immediate surgery.
- Fistulas and abscesses
- Colon carcinoma: Patients with ulcerative colitis have an increased risk of colorectal cancer. The risk increases significantly with increasing disease duration. For example, it is about 40 percent for 25 years of illness.
Ulcerative colitis can also cause colorectal cancer © peterschreiber.media | AdobeStock
The main complications of ulcerative colitis outside the colon are:
- Inflammations of the eye
- Inflammation of the bile ducts
- Joint pain, joint inflammation
- Liver damage
- painful skin lesions (erythema nodosum)
Treatment of ulcerative colitis
Since the causes for the development of ulcerative colitis are not known, the disease cannot be cured. Therefore, treatment aims to relieve the symptoms and reduce the risk of complications.
Depending on the severity and progression, there are different options available for the treatment of ulcerative colitis:
- In mild cases, usually drug treatment (e.g. immunosuppressants, cortisone, 5-aminosalicylic acid) and change of diet
-
In the case of a severe progression, complications or insufficient effectiveness of drug therapy, surgical treatment (ulcerative colitis surgery)