Sentinel piles are enlarged folds of skin in the anal region that are partially visible from the outside. The skin folds mostly consist of soft or sagging skin. However, they can also swell and develop hard lumps, especially in the case of chronic inflammation, heavy pressing due to hard bowel movements, or other pressure on the anal margin.
The causes for the development of these skin lesions in the anal area are only partially known. In general, diseases and conditions in which there is increased pressure in the rectal area (e.g., chronic constipation, pregnancy, childbirth) are risk factors for the development of sentinel piles. In some cases, they are a concomitant of the following proctological (rectum-related) diseases:
In general, skin flaps occur in about 60 percent of the population. On average, they are more frequent in women from the age of 20, and in men from the age of 40.
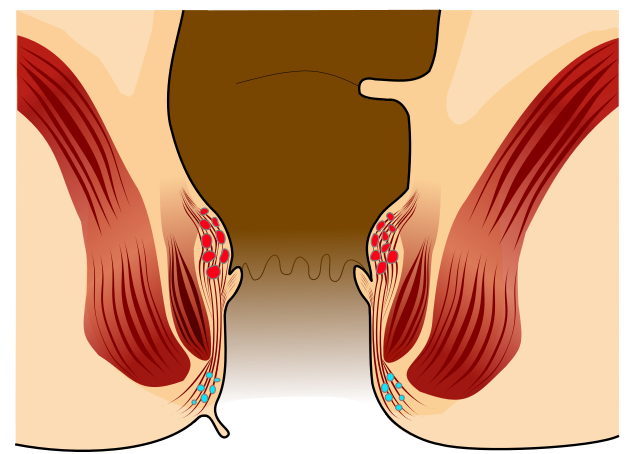
Anal skin tags are not infrequently confused by non-medical professionals and sufferers with enlarged hemorrhoids. However, they are different in terms of the clinical pictures. Hemorrhoids are annular vascular cushions under the rectal mucosa supplied by the arteries. They are not a disease, but ensure the contraction of the anus and continence, i.e., the controlled retention of bowel movements. Only a significant enlargement of hemorrhoids is pathological, especially when they emerge from the anal canal and are visible externally. In this context, doctors refer to it as hemorrhoidal disease.
Unlike hemorrhoids, anal skin tags are not vascular cushions, but merely saggy portions of the anal canal skin that has emerged outward. However, in the context of hemorrhoidal disease, the skin of the anal canal may be displaced outward. Accordingly, skin lesions on the anal margin may be an indication of an underlying hemorrhoidal disease. Sentinel piles can be a consequence of hemorrhoids.
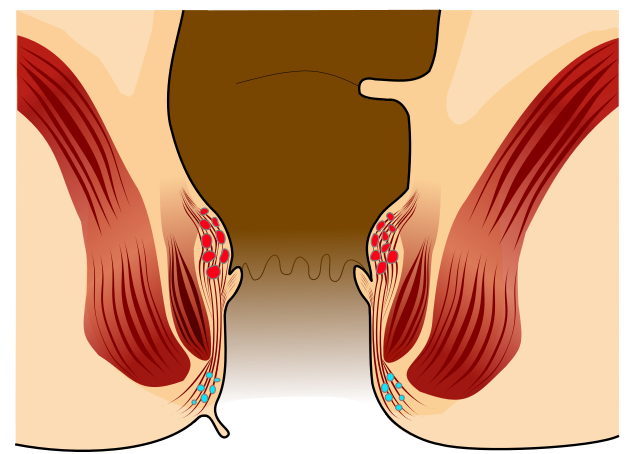
Sentinel piles (small folds) at the anus © Armin Kübelbeck, CC-BY-SA, Wikimedia Commons
Since anal tags are more common in conditions with increased pressure in the anal region, pregnancy and childbirth are considered important risk factors for developing sentinel piles.
Anal tags can develop especially after pregnancy or childbirth. In this case, women, especially those who have given birth several times, notice skin changes in the anus area. But even during pregnancy, anal tags can form as a result of hormonal changes, as the anal skin becomes softer and swells due to water retention. The additional pressure on the pelvic floor can cause parts of the anal skin to shift outward and form folds there. While the water retention regresses, the externally visible skin wrinkles remain after pregnancy in many cases.
Anal tags are generally harmless and usually do not cause any symptoms. Therefore, they are more of a hygienic and cosmetic problem.
However, if anal hygiene is severely compromised by the skin flaps, anal tags can also cause problems. This is because limited anal hygiene increases the risk of infections, for example, caused by bacteria or fungi.
In this case, typical symptoms caused by anal tags include:
- Itching,
- Burning,
- Skin rashes (perianal eczema)
- Sores on the anal canal, and
- Spotting, which may be visible on underwear or toilet paper.
Anal tags can be very easily diagnosed since they are diagnosed by a so-called "visual diagnosis". They are usually visible to the naked eye and can be diagnosed during an inspection (the medical term for an examination by simple observation) of the external anal region. Consequently, no further instrument-based examinations are necessary to diagnose sentinel piles.
However, as mentioned, sentinel piles are associated with other diseases of the rectum in some cases, so the anal and rectal area is still carefully checked. Thus, a digital examination (palpation with the finger) is recommended to be able to detect abnormalities. This may identify any additional hemorrhoids or hidden tears (anal fissures). Perianal hematomas, anal carcinomas, and benign connective tissue growths may also be associated with sentinel piles.
If palpation of the anal canal alone reveals suspicious findings such as palpable wall thickening, pain, or bleeding, an endoscopy of the rectum (rectoscopy) or the entire colon (colonoscopy) will be arranged.
Since sentinel piles are accordingly harmless, treatment is only necessary in rare cases. In any case, careful and at the same time gentle hygiene of the anal area is recommended. This means you should clean your anal region after your bowel movements using a damp washcloth or toilet paper. Use clean water and avoid soaps or disinfectants. Moist toilet paper can also cause skin irritation due to the preservatives and fragrances it contains. In addition, always dry the anal region gently.
In case of discomfort, a zinc ointment can be used for a short time. If anal eczema has developed, you can treat it with a hemorrhoidal ointment or oak bark as well as chamomile sitz baths. Consult a proctologist if your symptoms persist or do not improve. Surgical removal of the sentinel piles (sentinel pile excision) is recommended only in cases of difficult anal hygiene with secretion build-up and diseases of the anal skin. In this procedure, the skin flaps are removed with an electric knife under local anesthesia. In the rare cases in which sentinel piles
- Become painful,
- Are being pinched,
- Hinder bowel movements, or
- Lead to continence problems (bowel movements can no longer be held),
operational measures may also become necessary.
Even in the case of sentinel piles requiring surgery, no major complications are expected and the prognosis is very good. After the operation, postoperative bleeding may occur from the small blood vessels which, in most cases, disappears on its own.
Closure of surgical wounds is often accompanied by pain, as an infection (inflammation with a small area of pus) usually develops in the operated area and the wounds thus experience pressure. You will therefore be given a painkiller by your doctor. In case of excessive pain and swelling of the area operated on, antibiotic therapy is indicated.
During the operation, a wound dressing with a disinfectant and ointment is applied. You will continue this wound treatment (compress plus disinfectant and ointment) at home after surgery. You can additionally encourage wound cleansing and healing with the help of sitz baths and multiple daily showers.
One and four weeks after the procedure, the attending physician checks the progress of the wound’s healing. Signs of incipient healing should be visible after two to three weeks at the latest. After healing is complete, you will usually not be able to see any signs of the procedure. As a rule, you will be unable to work for two weeks. If adequate anal hygiene is not possible due to your job, the inability to work may last longer.
In principle, it is possible for anal tags to recur. This is true both in cases where sentinel pile surgery was performed, but also and especially without surgery. There is no silver bullet that can prevent anal tags. Nevertheless, it is possible to minimize the risk by taking measures to regulate the stool, getting plenty of exercise, and eating a healthy diet rich in fiber. Since a sedentary lifestyle and being overweight also increases the risk of developing anal tags, much can also be achieved by changing lifestyle habits accordingly. However, there is no guarantee.