An enlarged prostate is the most commonly diagnosed urologic disease in male patients. In the age group of 50 to 60-year-old men, one in two is affected.
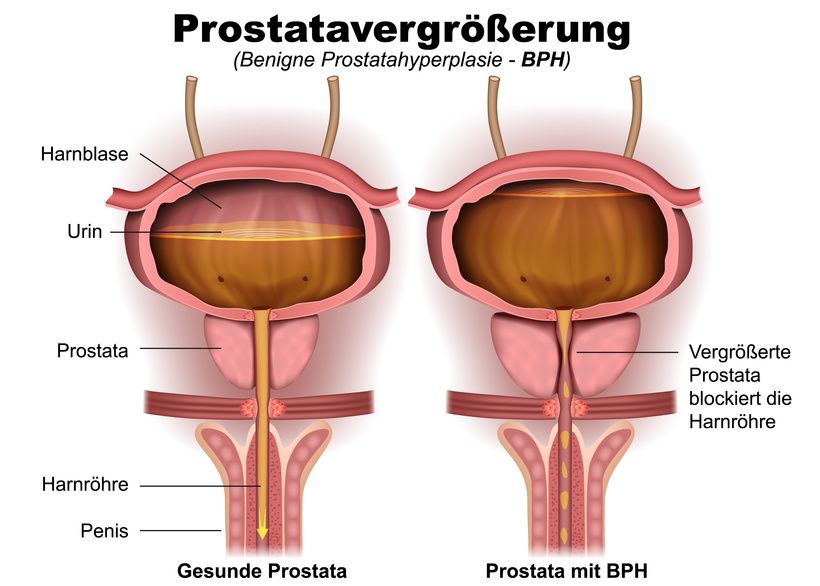
Increased growth of tissue cells in the prostate gland leads to an enlargement of the organ. Normally, the prostate weighs only 25 grams and is about the size of a chestnut. Due to cell growth, the prostate gland can then reach a weight of up to 150 grams.
However, the proliferating cells behave non-invasively, i.e., they do not grow into neighboring tissues. It is therefore a benign tumor.
The prostate is located under the urinary bladder directly in front of the rectum. Therefore, the enlargement of the prostate gland causes corresponding discomfort.
Benign prostatic hyperplasia cannot be prevented. However, with a healthy lifestyle and regular physical activity, you can reduce your personal risk of developing it. Important pillars of a healthy lifestyle are maintaining a normal weight and abstaining from nicotine.
In medical literature, the term prostate adenoma is more often found as a synonym for BPH. However, this is not medically correct: In benign prostatic hyperplasia, the number of glandular, muscle, and connective tissue cells increases. However, in an adenoma, there is only an increased number of glandular cells.
Enlargement of the prostate manifests mainly with the following symptoms:
- Weak urine stream up to urinary retention,
- Interrupted urine stream,
- Delayed urination,
- Pressing feeling during urination,
- Frequent urge to urinate, but there are only small amounts of urine,
- Nocturnal urge to urinate,
- Dribbling at the end of urination,
- The feeling that the bladder is not empty after urination is completed,
- Pain during urination (in individual cases), and
- Male impotence.
If you suffer from one or more of these symptoms, you should quickly consult a specialist in urology.
If you cannot urinate at all, go to a hospital emergency room as soon as possible. This leads to urinary retention up to the kidneys, which causes uremia. In urine poisoning, toxins from the urine pass into the blood, leading to the risk of mortal danger.
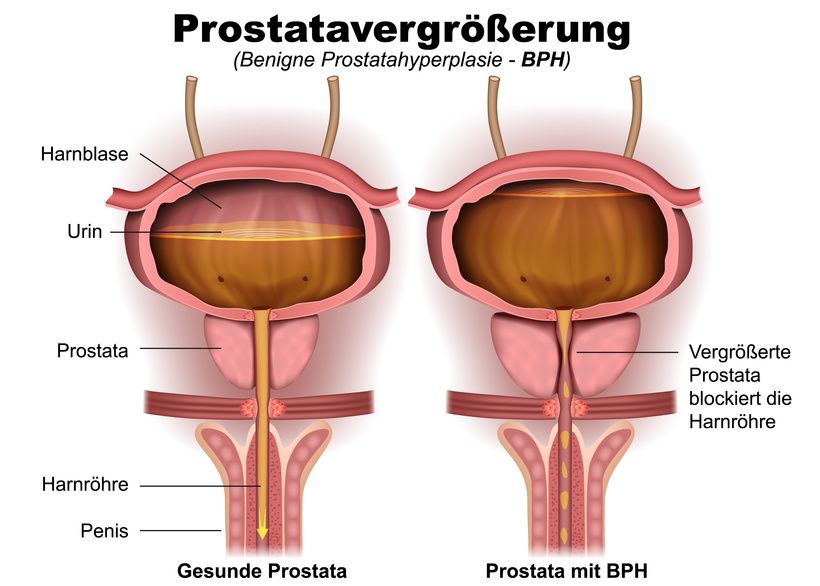
An enlarged prostate presses on the urethra, among other things, making it difficult to urinate © bilderzwerg | AdobeStock
Diagnosis begins with a digital rectal examination by a urologist. In doing so, the urologist inserts a finger into the patient's rectum and palpates the prostate gland. If the prostate is enlarged due to benign prostatic hyperplasia, it has a smooth elastic surface.
After that, the doctor checks the sphincter function and reflexes to rule out other diseases such as Parkinson's disease.
To rule out a possible urethral infection, the doctor has a urine sample from the patient tested in the laboratory. A tiny tissue sample from the prostate gland provides information about whether the cells are really benign or whether they point to prostate cancer. The tissue sample is obtained from the rectum.
The ultrasound image makes possible complications like diverticula (protrusions of the organ wall) and bladder stones visible. This is performed using a transrectal ultrasound (TRUS), which is inserted into the rectum of the patient. Conventional lower abdomen ultrasounds show the size of the prostate and the amount of residual urine.
With the help of an uroflowmetry, the strength of the urine flow is measured. In healthy patients, it is approximately 20 milliliters per second. However, if the amount is less than 10 milliliters, this is an indication of a narrowed urethra. During an uroflowmetry, the patient urinates into a funnel equipped with special sensors.
In certain cases, a cystoscopy is used to clarify the suspected diagnosis of benign prostate enlargement.
Prostate glands produce a secretion that protects sperm cells and stimulates them to increase their activity. The fluid is released into the urethra. The glands located in the prostate are surrounded by smooth muscle cells and connective tissue cells.
In benign prostatic hyperplasia, the number of muscle cells, connective tissue cells, and glandular cells increases greatly. According to current medical findings, this happens because the aging cells die off late. This makes the outer layer of the prostate thinner. In addition, the organ is no longer capable of producing sufficient secretion.
What causes cells to live longer than normal has not yet been fully understood by medical researchers. However, dihydrotestosterone (DHT) seems to play a key role. This is the variant of the male sex hormone testosterone that is more potent in the body.
The female sex hormone estrogen, which is also found in the male body, could also increase the likelihood of developing benign prostatic hyperplasia. It is found in higher concentrations in men after male menopause than in younger men, whereas DHT levels in the blood are lower. This increase in estrogen, in turn, increases the risk of developing benign prostatic hyperplasia.
A high proportion of fat cells in the body further increases the estrogen concentration in the blood. Therefore, men with severe obesity generally have a higher risk of developing prostate enlargement.
The space between the glands is also involved in the development of the disease: If it binds growth factors in excess, this promotes cell proliferation or prevents their natural death.
Prostatic hyperplasia usually has a genetic cause, but only in those patients in whom it develops in earlier decades of life. Physicians believe that only about 9% of benign prostatic hyperplasia cases in men over 60 are genetic.
If the disease does not yet cause any symptoms, it is sufficient to check it at regular intervals.
Drug therapy
In stage I of the disease or, in milder cases, in stage II, the patient is administered medication.
Among the most commonly taken remedies are herbal medications. They are very well tolerated, but can only be used for minor symptoms. These include, for example, medications with
- Nettle roots,
- Pumpkin seeds,
- Rye,
- African plum (Dacryodes edulis), or
- Saw palmetto.
They prevent the formation of growth factors, 5-alpha-reductase, which is the enzyme that converts testosterone into DHT, or cause cells to die more quickly. They also block the male sex hormone.
Alpha-blockers are synthetically produced drugs that relax the prostate and urethral muscles. Thus, they allow easier urination. This group of active ingredients includes, for example, tamsulosin, doxazosin, and alfuzosin.
Chemical 5-alpha-reductase inhibitors are the active ingredients dutasteride and finasteride.
Patients who are prescribed these drugs are more likely to experience potency problems and decreased interest in sex. For this reason, PDE inhibitors such as tadalafil have recently been preferred. They have a similar effect to the herbal enzyme blockers.
To reduce the strong urge to urinate, agents are used that inhibit the activity of the bladder muscle.
All medications used to treat benign prostatic hyperplasia slow the progression of the disease. Sometimes there is even shrinkage of the prostate.
Prostate artery embolization
Prostate artery embolization (PAE) was first performed in 2008, making it a fairly recent method. Nevertheless, it is increasingly becoming an alternative to drug therapy or a TURP (see below). It is a minimally invasive procedure that does not require general anesthesia and can be performed on an outpatient basis.
Recent studies show that prostate artery embolization has significantly fewer complications than a surgical procedure such as TURP:
- Low risk of infection,
- No bleeding and no secondary bleeding through the urinary tract, and
- No risk of incontinence.
The principle of prostate artery embolization is based on reducing the blood supply to the prostate. Doctors achieve this with the help of a catheter. It is inserted through a tiny puncture through the iliac artery into the prostate artery. Doctors check the position of the catheter during the procedure using computed tomography (CT). Tiny plastic particles are now inserted into the branching arteries of the prostate via the catheter until the blood supply is cut off.
The reduced blood supply may cause the enlarged prostate to shrink again in the weeks or months afterward. This gives the patient back his quality of life. Doctors record success in 75-94% of all procedures.
However, prostate artery embolization cannot always be performed. Various diseases are exclusion criteria, including
Surgical treatment
There are several surgical procedures for removing benign prostatic hyperplasia. The procedure that is ultimately used depends on the individual.
The gold standard is still transurethral resection of the prostate (TURP). The procedure is similar to a cystoscopy: The surgeon inserts a narrow tube into the urethra; it is equipped with a high-resolution camera and a light at the free end. The powered metal loop ablates the excess tissue layer by layer.
The technically improved TURP procedure used today only occasionally leads to undesirable side effects. However, the complication rate increases the larger the prostate is.
Transurethral incision of the prostate (TUIP) is only considered if benign prostatic hyperplasia is not yet too severe. Excess tissue is only cut at the junction between the prostate and the bladder neck so that the urethra is not constricted.
Another surgical method is transurethral microwave therapy (TUMT): The waves destroy the benign tissue with heat, causing the prostate to shrink.
Lasers are also used for an enlarged prostate. They destroy the prostate tissue or ablate it away, layer by layer. The HoLEP method in particular has a similarly high efficiency as the standard method.
Open surgery is necessary only in the case of a very severely enlarged prostate. The surgeon cuts open the bladder and removes the prostate gland from there (prostate enucleation).