Recommended specialists
Brief overview:
-
What is diverticulitis? A condition where protrusions of the large intestine wall (diverticula) become inflamed, especially between the descending colon and rectum.
-
Symptoms: Severe abdominal pain, indigestion, pressure-sensitive hardenings, and fever. A dangerous complication is intestinal perforation and bowel obstruction.
-
Causes and risk factors: Inflammation occurs when fecal stones and bacteria accumulate in the diverticula. Diet, smoking, being overweight, and certain underlying diseases increase the likelihood of developing inflammation.
-
Diagnosis: After the medical history and physical exam, a blood count and imaging procedures (ultrasound, CT scan) provide information. A colonoscopy cannot be performed if inflammation is suspected.
-
Treatment: Therapy depends on the stage of the disease. Conservative measures, such as a change in diet, may be sufficient for mild forms; for advanced stages, surgical intervention, in which the corresponding section of the intestine is removed, may be necessary.
- Prognosis: The progression of the disease can be completely different for different patients. Even after surgery, diverticula can reappear, possibly leading to diverticulitis. A healthy lifestyle is recommended for prevention.
Article overview
- What are diverticula?
- Symptoms
- Causes and risk factors
- Medical examination and diagnosis
- General information about diverticulitis treatment
- Therapy for acute uncomplicated diverticulitis (stage/type 1)
- Therapy for acute complicated diverticulitis (stage/type 2)
- Therapy for chronic diverticulitis (stage/type 3)
- Therapy for intestinal bleeding (stage/type 4)
- Diverticulitis surgery
- Progression and prognosis for diverticulitis
What are diverticula?
https://www.leading-medicine-guide.com/de/anatomie/darmDiverticulosis refers to protrusions to the outside (diverticula) in the intestinal wall in the area of the large intestine (colon). They represent a separate clinical picture. In diverticulitis, the diverticula are inflamed.
Most commonly, the diverticula occur in the left-sided portion of the colon, particularly in the sigmoid colon. The sigmoid colon is located between the descending colon and the rectum. However, diverticula can also occur in the other areas of the colon as well as throughout the rest of the gastrointestinal tract.
The presence of such diverticula in the colon is called diverticulosis so long as they don’t cause symptoms. However, if the diverticula then become noticeable through symptoms, this is referred to as diverticular disease.
Diverticula cannot regress.
In the case of a false diverticulum (pseudodiverticulum), only the mucosa lining the intestine protrudes out. Should this occur, the overlying wall layer, the submucosa, may also be affected.
By contrast, a true diverticulum is a protrusion of the entire intestinal wall. The video shows what the clinical picture in a colonoscopy looks like:
Symptoms
Diverticula occur in many people and their frequency increases with age. In most cases, diverticula are asymptomatic.
Symptoms only occur when the diverticula are inflamed, i.e., diverticulitis. They include
- Severe abdominal pain, especially on the left side,
- Digestive disorders (constipation, diarrhea, flatulence),
- Pressure-sensitive hardenings, and
- Fever.
The following dangerous complications may occur:
- Intestinal perforation: Tearing of the intestinal wall and leakage of air and feces into the abdomen, causing the inflammation to potentially spread to neighboring structures.
- Intestinal obstruction due to the thickening of the intestinal wall caused by inflammation.
Symptoms often occur in flare-ups.
The presence of diverticula in the intestine and their pathological changes can be divided into different stages:
- Stage/type 0 (asymptomatic diverticulosis): Diverticula are present that do not cause symptoms
- Stage/type 1 (acute uncomplicated diverticular disease/diverticulitis): inflammation of the diverticula without complications, i.e., the intestinal wall is not perforated (torn)
- Stage/type 2 (acute complicated diverticular disease/diverticulitis): Inflammation of diverticula with complications. Either the intestinal wall is freely perforated or covered perforated (that is, an abscess has formed)
- Stage/type 3 (chronic diverticular disease/diverticulitis): The disease is chronic and there are persistent or recurrent symptoms. Complications such as fistulas (connecting ducts) or stenoses (narrowing) may also develop
- Stage/Type 4: Diverticular bleeding
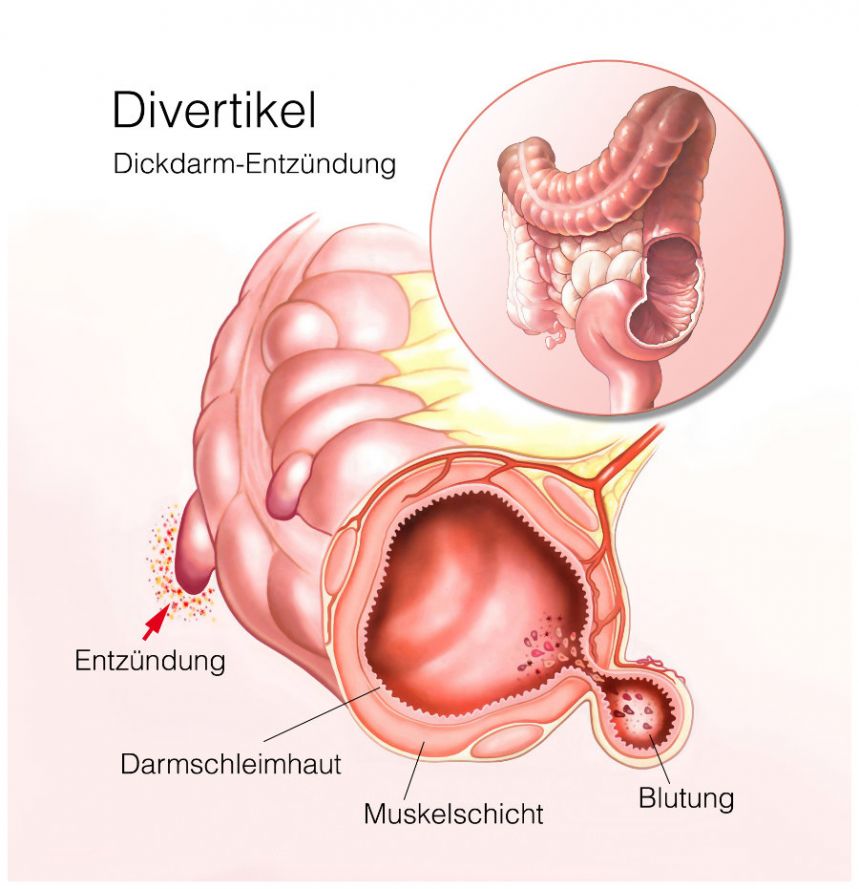
Illustration of diverticula in the colon © Henrie | AdobeStock
Causes and risk factors
The exact causes for the development of diverticula are not known. It is possible that certain stool characteristics, in addition to age, play a role in the development of diverticula. In particular, hard stools with a low-fiber diet and the resulting increased pressure in the intestine are considered risk factors.
Fecal stones and bacteria that collect in the protrusions can irritate and inflame the mucosa. The inflammation can spread the bacteria to adjacent structures such as the peritoneum, causing peritonitis. Fistulas and abscesses can also form.
According to the professional guidelines on diverticular disease, modifiable risk factors for the development of diverticulitis are
- Consuming red meat,
- Smoking,
- Being overweight, and
- Certain underlying diseases, such as arterial hypertension.
Medical examination and diagnosis
Besides
- A medical history (patient survey about symptoms, illnesses experienced, and medications taken),
- A blood test for elevated inflammation levels (C-reactive protein = CRP, leukocytes), and
- A physical exam (e.g., palpation of the abdomen and digital-rectal examination),
imaging studies are important for diagnosing diverticulitis. Thus, the diverticula can be depicted using an ultrasound examination and computer tomography (CT scan).
A colonoscopy should only be performed in an inflammation-free interval. In diverticulitis, there would otherwise be an increased risk of intestinal injury (perforation). Colonoscopies are used primarily to
- Clarify any diverticular bleeding and, if possible, staunch it immediately and
- Rule out malignant diseases.
General information about diverticulitis treatment
Specialists in internal medicine and gastroenterology (gastrointestinal diseases) and abdominal surgical experts in intestinal surgery are specialists in the treatment of diverticulitis.
Family physicians can treat most mild forms on an outpatient basis. Severe cases, on the other hand, must be treated as inpatients at special clinics for diverticulitis, usually clinics for gastroenterology or abdominal surgery.
Depending on the severity or stage of the disease, there are various treatment options. Conservative measures such as dietary changes, antibiotic therapy, and mesalazine administration are used for milder courses.
Surgical intervention is required for disease stages
- That do not respond to conservative measures,
- Where patients have experienced complications such as an abscess or intestinal perforation, or
- Where there is an increased risk of recurrence or complications.
Therapy for acute uncomplicated diverticulitis (stage/type 1)
Mild symptoms, such as irregular bowel movements, can often be successfully treated by regulating bowel movements.
Antibiotic therapy is not initially necessary for acute but uncomplicated diverticulitis. However, the prerequisite is that there is no increased risk of complications. Close monitoring of the patient is required though.
The risk of complications (perforations or abscesses) is increased in patients with various preexisting conditions, including
- Arterial hypertension (high blood pressure),
- Chronic kidney disease,
- Being under immunosuppression, or
- In case of allergic predisposition.
In this case, the doctor will prescribe antibiotic treatment. While taking antibiotics, the intestine should be "treated gently". Therefore, a low-fiber diet is recommended during treatment. After the inflammation has healed, it should be switched back to a high-fiber diet.
Therapy for acute complicated diverticulitis (stage/type 2)
Patients with acute complicated diverticular disease/diverticulitis should be hospitalized.
If there is no improvement with antibiotics, surgery should be performed. Abscesses can usually be drained by puncture or drainage.
Severe courses must be operated on immediately by an experienced abdominal surgeon (emergency surgery). A more severe course occurs with intestinal perforation or peritonitis (inflammation of the peritoneum).
Even patients at this stage who have been successfully treated with antibiotics are advised to undergo surgery during the inflammation-free phase.
Therapy for chronic diverticulitis (stage/type 3)
Under certain circumstances, it may be advisable to surgically remove the bowel segments containing the diverticulum during an inflammation-free interval. Removal is advisable, especially in cases of recurrent diverticulitis, but also in cases of frequent mild inflammation.
Stenoses are operated on when the narrowing obstructs the passage of stools. Fistulas should also be treated surgically.
New studies show that the quality of life in patients with recurrent inflammation improves significantly more after surgery than the regular use of antibiotics.
Therapy for intestinal bleeding (stage/type 4)
Most intestinal bleeding stops on its own. If this is not the case, it must be staunched. This can be performed either
- In the course of a colonoscopy,
- Angiographically (i.e., via a blood vessel), or
- Surgically.
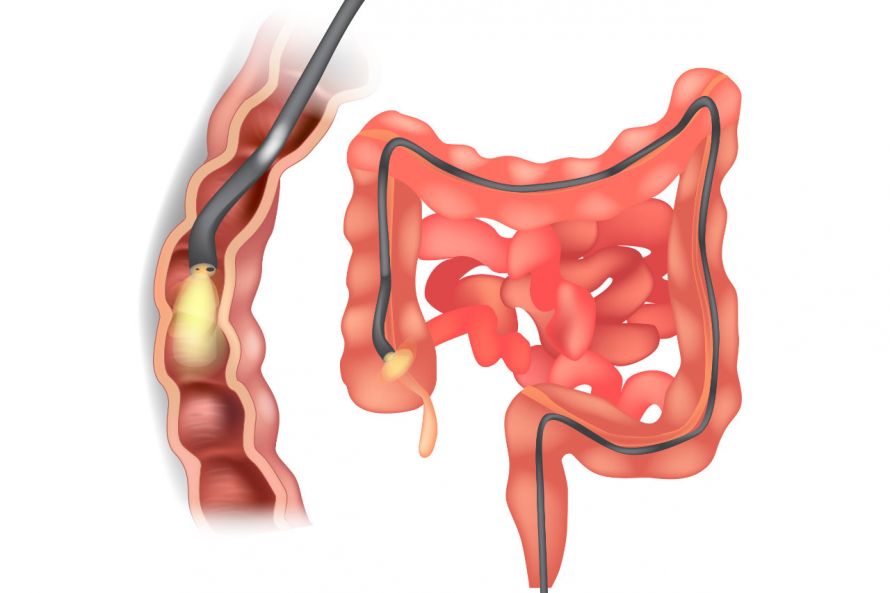
Procedures can be performed during a colonoscopy © sakurra | AdobeStock
Diverticulitis surgery
Surgical diverticulitis treatment involves sigmoid resection. This means that
- The intestinal segment containing the diverticulum (usually the sigmoid colon) and/or
- The rectosigmoid transition of the colon
is/are removed. If possible, this operation is performed as a minimally invasive procedure.
If perforation and peritonitis have already occurred, an open surgical procedure is chosen for treatment more often.
The creation of a stoma (artificial rectal opening) is not necessary in most cases today.
Progression and prognosis for diverticulitis
Diverticulitis can take very different courses. Inflammation of the diverticula often occurs in flare-ups. This means that after the symptoms have subsided, inflammation occurs again. Depending on the severity, between two and 35 percent of patients with diverticulitis are affected.
Most patients with diverticula remain asymptomatic. However, in some, bowel perforation may occur as part of the first episode of the disease. In contrast, other patients do not develop complications even with recurrent flare-ups.
The risk of bowel perforation is greatest during the first episode, and then decreases with each subsequent episode. However, the risk of another flare-up also increases with each recurrence.
After sigmoid resection, diverticula or diverticulitis may develop again in other parts of the intestine.
- Regular physical activity,
- Adequate fluid intake,
- Maintaining a normal weight, and
- A high-fiber vegetarian diet
are recommended for the prevention of diverticulitis.