Recommended specialists
Article overview
Hip prosthesis - Further information
Overview of hip prosthesis
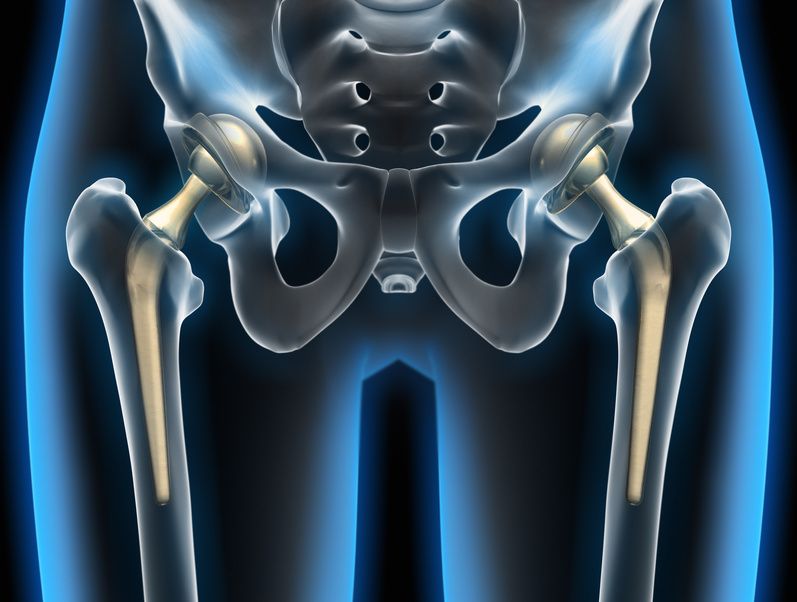
Hip prosthesis, or hip replacement surgery, is a procedure that replaces a damaged ‘ball-and-socket’ hip joint with a new, artificial hip joint, designed to operate in the same way as the bone and cartilage structure of the natural joint.
When disease or injury damages a hip joint or thigh bone, this can cause pain and loss of mobility, which may affect walking and the routine tasks of everyday living. If pain-relieving medications, physical therapy, braces or supports prove ineffective, your doctor may suggest a joint replacement, using a hip prosthesis procedure.
Who offers hip prosthesis?
Hip prosthesis surgery is commonly offered by specialist private health clinics, which are in some cases managed by universities, insurers, mutual societies or religious institutions. In addition, there are state-run hospitals (such as those managed by the UK’s NHS or Germany’s Federal Ministry of Health), which also employ skilled surgeons who specialise in various kinds of hip prosthesis surgery.
What does hip prosthesis help with?
A hip prosthesis can help with a range of conditions that can damage the hip joint and therefore require hip replacement surgery. These may include:
- osteoarthritis, a condition that attacks the slick cartilage material covering the ends of bones, which is designed to allow smooth movement of the joint components
- rheumatoid arthritis, a condition in which an overactive immune system causes inflammation and deformities in bone and cartilage joints
- osteonecrosis, a condition that develops if there is reduced blood flow to joints, and sometimes leads to bone collapse and deformities
A hip replacement may be recommended if you experience pain that:
- continues even when treated with medication
- gets worse when you try to walk, even with a stick or a walker
- interrupts your sleep pattern
- impedes your ability to negotiate stairs and steps
- impedes your ability to rise from a sitting position
When is hip prosthesis used?
A hip prosthesis procedure is recommended if non-surgical treatments have failed to address your pain and mobility needs. During the procedure, the surgeon will:
- create an incision at the front or side of your hip
- remove all damaged and diseased cartilage and bone to expose a new and healthy bone layer
- install the prosthetic socket in your pelvic region to replace your damaged socket
- install a prosthetic ball (attached to a stem) which is fitted into your thighbone
What are the risks of hip prosthesis?
There are some particular risks associated with hip replacement surgery:
- blood clotting can cause a clot to form in a leg vein, which may possibly circulate and reach the lung, heart or brain, causing serious difficulties. Blood-thinning agents may be used to reduce the risk.
- infections can occur in your surgical wound as well as in deeper tissues. Any significant infection near your new hip joint may compromise the surgery and require another replacement.
- fractures may occur during surgery, and perhaps require metal supports or even bone grafts.
- dislocation can occasionally happen with over-extended movements of your new joint. This may require a brace, or perhaps further surgery, to stabilise the new hip joint.
- a change in your leg length could become apparent after surgery. This sometimes results from a muscular weakness in your hip area. Gradually building up muscle strength, accompanied by stretching exercises may help to overcome this problem.
- looseness can develop in your new joint and cause further pain, which may require corrective surgery.
A further hip replacement
If in place for a number of years, a prosthetic replacement hip may eventually wear out and require another replacement. Modern prosthetic joints are now made from more durable materials and thus should last a lot longer.
Metal-to-metal complications
Though now very rarely fitted, any prosthetic hip joint with a metal cup liner poses a further problem of metal-to-metal contact. This type of structure can cause the release of metal ions into the bloodstream, possibly resulting in inflammation and presenting a risk of bone erosion.
Are there alternatives to hip prosthesis?
In some circumstances, hip resurfacing may be available as an alternative surgical procedure to a hip prosthesis. During hip resurfacing, only the damaged bone surfaces of your hip joint are removed and replaced with metal. The benefit of this procedure is that much more of your natural bone is preserved. Nevertheless, hip resurfacing may not be a suitable option for:
- post-menopausal women, who may be prone to osteoporosis (weak and brittle bones)
- any adult over 65 years of age, whose ageing bones will be weakening
Hip resurfacing is now less in favour because of some concerns that the metal may cause further soft tissue damage in the hip region.