The liver is a large organ that sits in the upper right area of your abdomen, just below the ribs. Though several cancers can develop in the liver, hepatocellular carcinoma, which begins in the most abundant type of liver cell (hepatocyte), is the most common form. Other liver cancers, such as intrahepatic cholangiocarcinoma and hepatoblastoma, occur much less frequently.
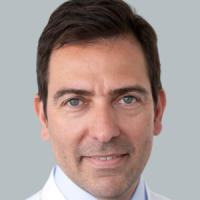
Recommended specialists
Article overview
Overview of liver cancer
Some cancers that have an impact upon the liver actually begin elsewhere in the body, before spreading to the liver through the bloodstream or via the lymphatic system. These are known as metastatic cancers, and each one is named according to the area of the body where the cancer originated. Thus, metastatic lung cancer begins in the lungs, before spreading to the liver.
Many more cancers spread to the liver as a secondary site than originate there.
Symptoms of liver cancer
For some people there may be no symptoms during the early phases of liver cancer. But when they do develop, the symptoms may include:
- tenderness, discomfort and pain in the upper abdomen
- jaundice (a yellow discolouration of the skin and the whites of the eyes)
- white, chalky stools
- nausea
- vomiting
- bruising or bleeding easily
- weakness and fatigue
Causes of liver cancer
Viral infection with hepatitis viruses remains one of the most common causes of liver cancer, but in many instances, the root cause remains unclear.
Liver cell DNA can mutate (change) and cause the cells of the liver to grow and mass together to form a cancerous tumour.
Diagnosis of liver cancer
A liver cancer diagnosis starts with a physical examination, plus a full medical history.
Further diagnostic tests and procedures that may then be called upon include:
- liver function tests, which help to assess the health of your liver
- CT or MRI scans of your abdomen to create detailed images of the liver and nearby organs
- a liver biopsy, which removes a small liver tissue sample for laboratory analysis
- a laparotomy involves a small incision, which allows a tiny camera to view your liver and surrounding organs, and perhaps collect samples for analysis
If a liver cancer is discovered, your doctor will evaluate the progress and extent of the condition. The most advanced stage of a liver cancer is described as stage four.
Treatment of liver cancer
Any proposed treatment for liver cancer will take into account:
- the number of tumours, plus their size and location
- how well the liver presently functions
- whether cirrhosis (scarring) has occurred
- whether the cancer has spread to other organs
Liver cancer treatment options may include:
- hepatectomy, which removes part or all of the liver – an option where cancer is present in the liver only
- a liver transplant inserts a healthy liver in place of the diseased organ – only possible if the cancer has not spread
- ablation is a procedure that eradicates cancerous cells under local anaesthetic – an option for those who are not eligible for surgery or a liver transplant
- chemotherapy is a drug therapy that destroys cancerous cells – this procedure can be delivered via an outpatient clinic
- external radiation therapy uses a powerful radiation beam to eliminate cancer cells
- internal radiation therapy injects small radioactive spheres, which close off the hepatic artery to reduce the blood supply to a tumour, while allowing the portal vein to continue supplying the liver with blood
- targeted therapy selectively delivers medication to destroy cancer cells and thus inhibit and decrease tumour growth – another option for those who are not eligible for surgery or a liver transplant
- embolization and chemo-embolization are surgical interventions designed to close off the hepatic artery and reduce the blood supply to the tumour
Chances of recovery from liver cancer
For those with localised liver cancer, the five-year relative survival rate is around 31%. In addition, for those with regional stage liver cancer, which means the cancer has spread to other organs close by, the five-year relative survival rate is around 11%.
Prevention of liver cancer
Not all liver cancers are preventable. However, your risk of developing liver cancer can be significantly reduced by taking measures that will prevent the development of conditions that are often associated with liver cancer.
Lower your risk of cirrhosis (scarring of the liver) by:
- achieving and maintaining a healthy weight
- consuming only moderate amounts of alcohol (if any)
Get yourself vaccinated against hepatitis B.
Adopt safe measures to prevent hepatitis C, and lower your risk of infection by:
- using protection and adopting safe sex practices
- avoiding using drugs, especially intravenous drugs, or at least using a sterile needle
- taking care to use only clean, professional shops for tattoos or piercings