Around a child’s first year of life, they begin their first attempts to stand and walk. An altered foot shape is then evident in children affected by flat foot. Medically, this is referred to as a planovalgus deformity; colloquially, it is known as a flat foot.
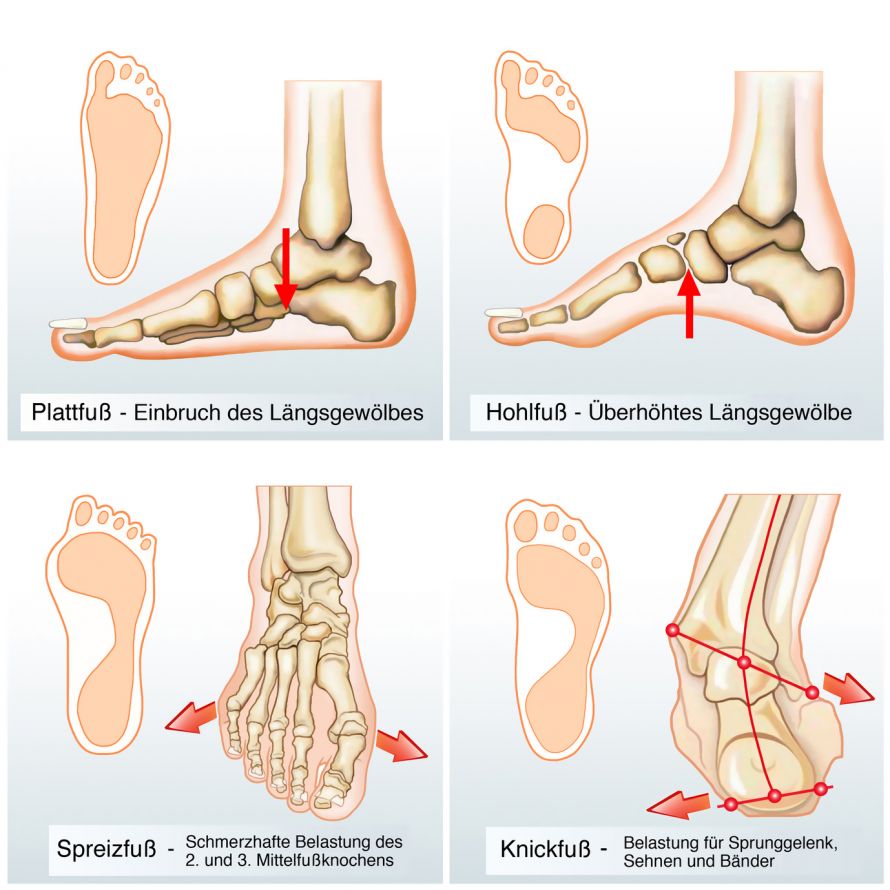
There are different changes in the foot’s anatomy, as shown in the graphic
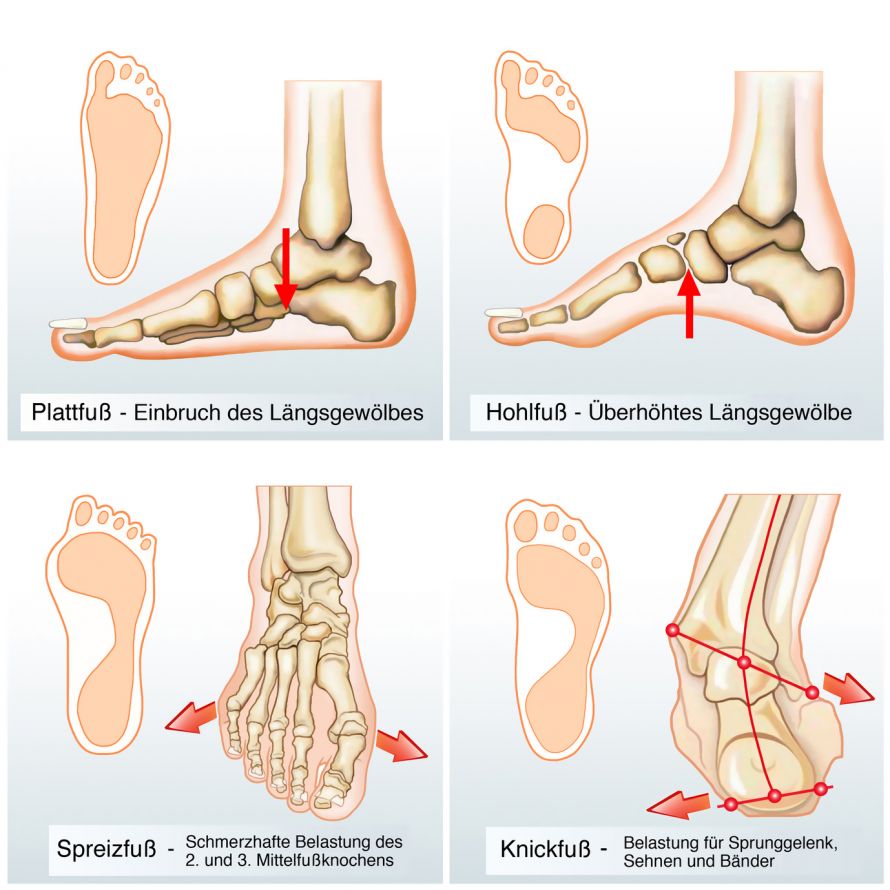
Different types of foot deformities © Henrie / Fotolia
Valgus, meaning bent out in Latin, refers to an increased bending above the heel (viewed from top to bottom and from behind) towards the outside of the foot compared to normal feet. Plano, meaning flat, refers to the flattening of the foot’s longitudinal arch normally present on the medial side.
The cause is often hereditary connective tissue or muscle weaknesses. Being overweight may also play an additional role, especially, in older children. In rare cases, paralysis can be the trigger.
Especially in young children, it is sometimes difficult to differentiate normal, age-correlated findings from a diagnosis. Flat foot often does not cause any symptoms either.
Between the ages of two and five, a slight planovalgus deformity is developmentally normal and usually does not need to be treated.
The misalignment is usually flexible, i.e., the foot shape can be passively influenced by the examiner. This is no longer possible in the case of a rigid planovalgus deformity.
Experienced specialists, such as orthopedics specialists or pediatric orthopedists diagnose flat foot by inspection and functional testing. If the findings are very pronounced, an x-ray examination is also beneficial.
With suitable equipment (podoscope), the footprint (podogram) can also be shown and assessed in specialist practices.
The most common form of flat foot is the flexible, low to moderate-grade flat foot of young children. It usually does not require any special treatment.
Semi-annual follow-up examinations are sufficient. The child should go barefoot a lot and be encouraged to do playful exercises that strengthen the foot muscles. This includes, e.g., standing on tip-toe, exercises for gripping with toes, etc.
In more severe cases, physiotherapeutic co-treatment may be advisable.
Orthotics are indicated only in cases of severe planovalgus deformity. They must be made according to plaster casts and produced by the orthopedic technician in consultation with the treating orthopedist. The wearing duration should not be too short and can be up to several years.
Their necessity must be regularly checked by the orthopedist.
Severe types of flat foot may warrant an indication for surgery. Prerequisites for this are
- Previous conservative treatment that was long-term yet unsuccessful,
- A correspondingly pronounced clinical finding, and
- Severe pain that is load-dependent.
A variety of soft tissue interventions (such as tendon transfers) are known. The common principle is to improve the muscles lifting the arch.
Performing such interventions should only be considered after the age of 8.
In the most severe progressions, especially in rigid cases, surgery on the foot skeleton may even be necessary. This is particularly necessary in the case of underlying neurological diseases such as infantile cerebral palsy. The surgery may include such things as reinforcing the arch with a bone wedge implant or inserting arch-supporting implants.
The most common form of flat foot, the flexible variant of early childhood, has a good prognosis. Most planovalgus deformities do not require special therapy. They often balance out again by school age due to normal growth.
The outcome of surgical procedures improves the more carefully the strict and individual indications for surgery are made.
In severe forms of flat foot that cannot be treated in any other way, it is often not possible to establish a complete physiological foot position. In most cases, however, surgeons achieve a worthwhile improvement of the misalignment, which alleviates the symptoms of those affected.
Particularly in cases of the common planovalgus deformity in young children without underlying additional diseases, sports have a positive effect on coordination and muscle strengthening, provided they are practiced within reasonable limits and in a fun way. Doctors generally recommend such sports activities.