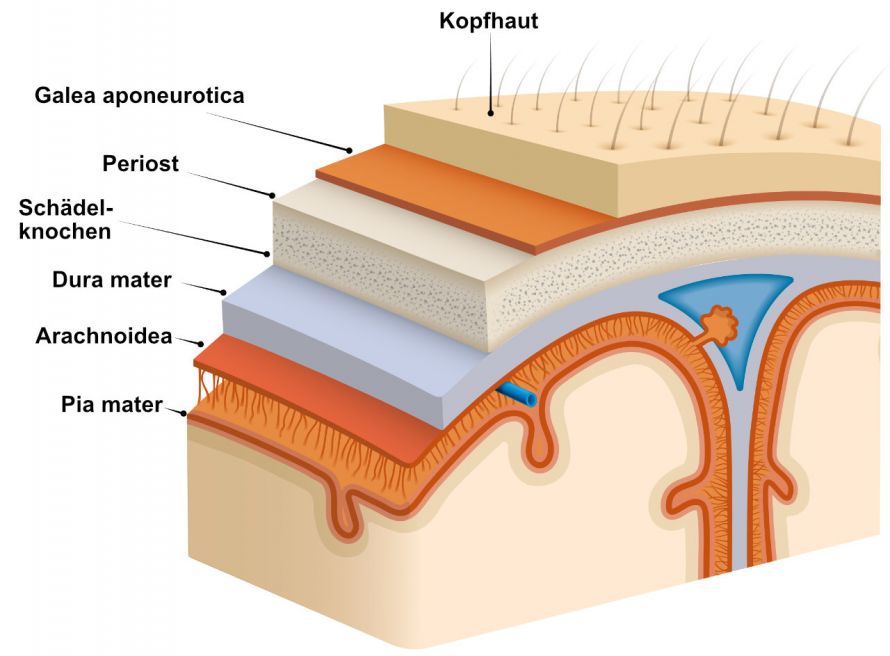
Most brain tumors develop from the actual brain substance. Meningioma, on the other hand, develops from the cells of the meninx. The meninx consist of three layers. A meningioma affects the arachnoid, the middle layer. The cells of this meningeal layer then grow uncontrollably.
Why the growth of these cells gets out of control has not yet been fully explained.
However, researchers have identified risk factors that favour the development of meningioma. This includes
- radiation for the treatment of a previous cancer,
- dental X-ray diagnostics (depending on the X-ray procedure used and the time at which the diagnostics were performed),
- the hereditary disease Neurofibromatosis type two. People affected by this are much more likely to develop a meningioma. Often, even several meningiomas form, while people without this hereditary disease only develop one tumor.
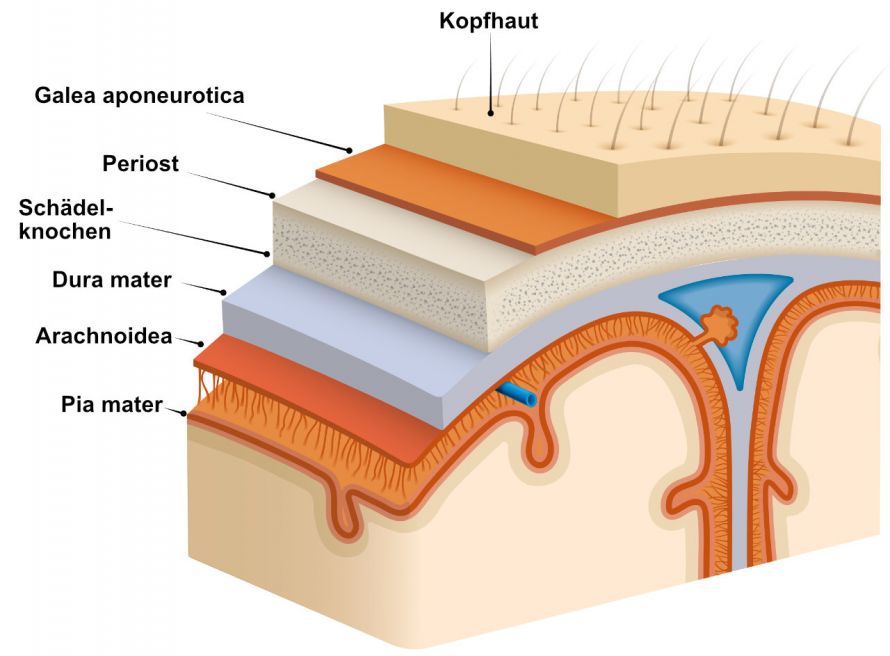
Meningiomas form in the arachnoid, the middle meningeal layer © olgadanilina | AdobeStock
A meningioma grows very slowly, so that the first symptoms often appear years after the onset of the tumour. It is only when the tumour mass reaches neighbouring brain regions or displaces nerve structures that symptoms occur. However, these are extremely non-specific and can also occur in other diseases.
If the tumour is located near the centre of movement, patients suffer from paralysis of the arms and legs.
Meningiomas, on the other hand, which are located in the olfactory groove of the brain, result in a restriction or loss of the sense of smell. However, since odour disorders tend to develop gradually, they often go unnoticed.
A meningioma can also irritate the three meninges and cause a seizure. Patients lose control of their body for a short period of time and suffer from twitching and cramps. They may also lose consciousness.
The tumour increases the pressure inside the skull. Increased intracranial pressure manifests itself through various symptoms. These include:
If the meningioma occurs on the meninges in the area of the spinal cord, the so-called local compression syndrome occurs. The patients complain of sensory disturbances and pain in the corresponding supply area. A significant mass in the spinal canal leads to myelopathy. Depending on the localisation, this manifests itself as
- Gait disturbances,
- Sensory disturbances and
- Disturbances when going to the toilet.
In some circumstances, the meningioma grows so slowly that the brain can adapt to the structural changes. These asymptomatic brain tumours are discovered by chance during a computer or magnetic resonance imaging.
Various imaging techniques can be used to diagnose meningioma. The most commonly used procedure is magnetic resonance imaging (MRI). This allows the different soft tissue qualities to be easily recognised and the examination does not require radiation exposure.
This examination method is also almost exclusively suitable for examining the spinal canal.
A more detailed classification of the space-consuming processes in the brain is possible with the aid of
- magnetic resonance spectroscopy (MRS),
- diffusion-weighted MRI and
- blood flow measurement of the brain.
Despite the indications provided by the imaging methods mentioned above, only the examination of tissue samples can confirm the diagnosis. This is especially important when a brain tumor first appears. For this purpose, tissue mass is removed from the tumour during an operation and then examined in the laboratory.
Not every meningioma requires treatment. A small tumour that does not cause any discomfort can be observed for the time being. Patients therefore have to see the radiologist at regular intervals. The radiologist uses CT or MRI to check whether the tumour is growing or remains unchanged.
If, on the other hand, the tumour causes symptoms, neurosurgical removal is advisable. In the case of a particularly vascular tumour, an embolisation is necessary before surgery. In the process, the blood vessels are closed to reduce the risk of major blood loss during the surgical procedure.
If the meningioma cannot be removed completely, it is followed by radiotherapy. This involves the use of high doses of ionising radiation. It is supposed to damage the genetic material of the tumour and thus prevent it from growing.
Another treatment option is the gamma knife: This radiosurgical radiotherapy device concentrates rays into a single point and destroys the focus of the disease.
The prognosis of the brain tumour depends mainly on the severity of the disease.
A grade I meningioma can usually be completely removed in one operation and therefore has a good prognosis.
About ten percent of all meningiomas are grade II. They can grow faster than grade one meningiomas and often grow back after a successful operation.
Grade III meningioma is classified as malignant. Unlike grade I and II tumours, it can also metastasise to other organs. The chances of a cure are low here and the prognosis correspondingly poor.
Overall, the 5-year survival rate of meningioma is more than 90 percent. This means that 90 percent of patients are still alive five years after being diagnosed.