Recommended specialists
Brief overview:
- What is skin cancer? A malignant cancer of the skin which can manifest itself in various forms.
- Types: A distinction is made between benign and malignant tumours. The prognosis depends on this classification. Benign skin cancers include basaliomas (basal cell carcinoma) and squamous cell carcinomas. In addition, there are precancerous lesions.
- Symptoms: Depending on their form, tumours of the skin can develop different symptoms. These include raised, sometimes nodular growth with discolouration of the skin, itching, oozing, bleeding, crusting.
- Causes and risk factors: UV radiation (solar radiation), sunburns in earlier years, regular visits to solariums, X-rays, an older age.
- Diagnosis: Using a dermascope, a doctor can often already detect a tumour. The ABCDE rule helps with classification. After removing the suspicious area, the tissue is examined histologically. If necessary, further imaging procedures are used.
- Treatment: The therapy depends on the classification. In the case of skin cancer, the tumour should be removed completely. Under certain circumstances, radiotherapy and chemotherapy may also be necessary.
- Prognosis: If skin cancer is treated at an early stage, it can often be completely cured. If it has already metastasised to other organs, the chances of cure decrease.
- Prevention: Protection from intense sunlight is the most important measure, especially for children. Sunburns should be avoided.
Article overview
Types
Mostly benign, only rarely malignant
Not every red spot is skin cancer. On the human skin there are a large number of differently coloured and differently shaped spots. Most of them are benign.
Malignant (malignant) tumours have the ability,
- to grow into neighbouring tissue (invasive growth) and
- to reach other organs via the bloodstream and form metastases there.
Benign tumours do not have this ability. In rare cases, however, a benign skin tumour can develop into a malignant skin tumour (skin cancer).
Benign skin tumours or skin lesions include for example
- the various forms of so-called epithelial and melanocytic nevi (including moles, freckles, liver spots),
- but also various cysts of the skin and
- seborrheic keratosis (also known as seborrheic wart, brown wart or senile wart).
Seborrheic keratosis is the most common tumour of the skin.
Not all types of skin cancer are the same
In the case of malignant skin tumours, a general distinction is made between basal cell carcinoma and malignant melanoma.
The two most common forms of basal cell carcinoma are:
- Basaliomas also known as basal cell cancer.
- Squamous cell carcinoma also known as SCC, pinocellular carcinoma or spinalioma. These skin cancers are relatively rare and usually develop from actinic keratoses (also known as solar keratoses). These are among the most common skin lesions.
Malignant melanoma is also known as melanoma.
Pre-cancerous lesions
Melanoma is thought to develop from benign nevi (moles). However, there are no reliable findings on this yet.
Basal cell carcinoma, on the other hand, develops on inconspicuous skin, i.e. it has no preliminary stage.
Frequency
The incidence of malignant skin tumours has been steadily increasing for several decades, so that skin cancer is now one of the most common cancers in humans. In total, about 19,000 people in Germany get malignant melanoma and about 200,000 people get basal cell carcinoma every year.
Malignant melanoma in particular, which accounts for about 4 percent of all new cancer cases in Germany and is responsible for about 1 percent of all cancer deaths, is very dangerous.
Symptoms
Basal cell carcinoma mainly occurs on parts of the body that are particularly intensively or permanently exposed to the sun. This includes
- the face (nose lips, ear forehead, etc.),
- the scalp,
- Neck and nape and
- the forearms and backs of the hands.
However, it can also occur in regions that have only been exposed to the sun from time to time.
Malignant melanoma, on the other hand, often occurs on skin areas that were repeatedly affected by severe sunburns in childhood and adolescence. In principle, however, it can develop in all areas of the skin, including
- the hairy scalp,
- the mucous membranes of the eye,
- in the mouth,
- on the genitals (penis, testicles, vulva) as well as on the
- foot (also sole of foot) and
- nails (toenail and fingernail).
The often inconspicuous basal cell carcinoma
Basal cell carcinoma usually appears at the beginning as a skin-coloured to grey-white hardening a few millimetres in size. It is growing very slowly but inexorably. This can cause the basal cell carcinoma to expand greatly and destroy all adjacent tissues. Depending on its shape, it can extend superficially or in depth.
Some types grow ulcer-like or flat, while others are nodular, scarred, look like eczema and/or itch. However, metastases rarely form.
Scaling actinic keratosis and nodular squamous cell carcinoma
The dermatologist identifies actinic keratoses by inspecting and palpating/touching the skin. They are only a few millimetres in size, sharply defined and have a rough, scaly and slightly reddened surface. In the course of time, brownish-yellow cornifications form, which are easy to scrape off.
Most of the time, actinic keratoses do not cause any symptoms. Sometimes there is
- Itching,
- Touch sensitivity or
- Inflammations.
Squamous cell carcinomas often develop at the base of these cornifications as nodular, fast-growing changes. They break open in the centre and can also form metastases.
Malignant melanoma is also known as cutaneous melanoma.
Melanoma is also characterised by its diverse manifestations: The skin lesions are often
- brownish to reddish-blue,
- blackish or grey-white and
- often asymmetrical.
In addition, it may ooze and form crusts. As it progresses, it can spread nodularly or superficially. If it grows in depth, the melanoma can form metastases in other organs relatively quickly.
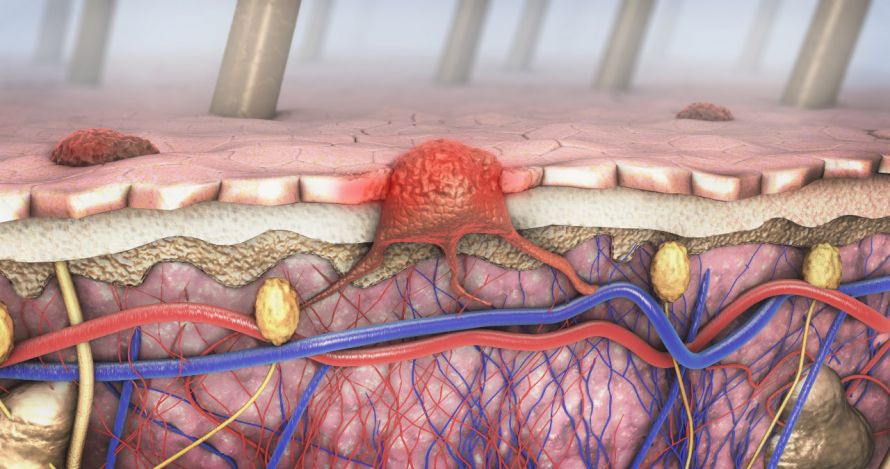
Malignant melanoma can grow into the blood vessels and spread cancer cells to other organs © Christoph Burgstedt | AdobeStock
Take skin changes seriously!
If you notice any changes in your skin, be sure to talk to your doctor about it.
Characteristics and signs of skin cancer:
- The skin patch bleeds or itches.
- The structure and surface of the skin patch changes.
- Crusts form.
- The skin patch becomes larger.
- The skin patch changes colour.
These changes and symptoms do not have to mean that a skin patch is skin cancer. However, it must be taken seriously and examined by an experienced dermatologist.
Causes and risk factors
UV radiation as the main risk factor
Solar radiation, or more precisely UV radiation, is considered the main risk factor and cause for the development of skin cancer or its precursors. UV radiation causes damage to the genetic material, the DNA. This can lead to uncontrolled growth of the cells and eventually to skin cancer.
There are studies that indicate that regular visitors to sunbeds have an increased risk of skin cancer. The risk of skin cancer is particularly increased in people who have visited a solarium for the first time under the age of 20. Since the skin of children and adolescents is particularly at risk, there is a ban on tanning salons for minors in Germany.

Regular visits to solariums increase the risk of skin cancer © didesign | AdobeStock
Since skin cancer usually develops over many years, age is also a risk factor. The likelihood of skin cancer increases with age. The risk is particularly increased if certain areas of the body have repeatedly had intensive contact with UV radiation. If you have had frequent sunburns in the past, you have an increased risk of skin cancer.
Also X-rays as well as some chemical substances can cause skin changes that can develop into skin cancer. Substances include
- Arsenic,
- Tar and
- some cytostatic drugs.
Immunosuppressed patients and those with certain pre-existing genetic conditions are also at increased risk of skin cancer. Especially in the case of malignant melanoma, there are indications that it is also hereditary.
Risk groups
The following groups of people are particularly at risk:
- Children (especially babies) and adolescents
- People who tend to sunburn quickly
- People with light skin, light or red hair or many lentigines (sunburn spots, age spots)
- People who have either many, conspicuous or congenital birthmarks/liver spots
- Immunosuppressed persons, for example after organ transplantation
- People who have already had skin cancer themselves or who have first-degree family members who have already had skin cancer
- People who work outdoors or who spend their leisure time in the sun
Examination and diagnosis
Due to this variety of possible manifestations of skin cancer, clarification by an experienced specialist is absolutely recommended. Unfortunately, supposedly harmless eczema or moles turn out to be skin cancer time and again.
Skin cancer prevention (skin cancer screening)
You should have your skin looked at by an experienced dermatologist at regular intervals. In Germany, the statutory health insurance covers the screening costs for this cancer screening every two years.
Shorter screening intervals are recommended,
- if you belong to a risk group, for example you have a lot of moles, and
- you have already been diagnosed with skin cancer in the past.
At the beginning of the examination, you should point out to the dermatologist any skin changes that you or your relatives have noticed. Also tell him if an area of skin is itchy, feels rough and scaly or has bled.
The dermatologist usually uses a special magnifying glass, a dermatoscope, for the subsequent examination of the skin. With the help of this illuminated magnifying glass, the dermatologist can take a closer look at suspicious areas. Often it is then already possible to say whether it is only a harmless skin change or not.
In some cases it is useful to take a photo of a skin lesion. This makes it easier to detect changes in a skin patch at the next check-up.
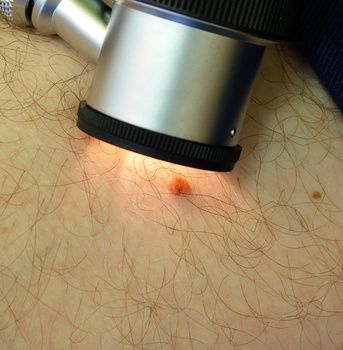
Examining a suspicious skin abnormality with a dermatoscope © Keith Frith | AdobeStock
Melanomas can be distinguished from other skin changes using a special procedure, confocal laser scanning microscopy. However, the costs for this examination are not covered by the statutory health insurance funds.
Malignant melanoma or not – the ABCDE rule
The dermatologist can also use the so-called ABCDE rule to make an initial assessment of whether it is a melanoma. The letters stand for the first letters of the English words for the characteristics of the skin change that are indicative of melanoma:
- A (asymmetry): The skin change is unevenly shaped (not round); the texture is heterogeneous.
- B (border): The skin change is irregular, partly sharp, partly blurred.
- C (colour): The colour of the skin change is brown, black, blue, red, white or grey; the pigmentation is inconsistent.
- D (diameter): The skin change has a size of more than five millimetres.
- E (elevation or evolution): The skin change protrudes above the skin level or increases in size.
You can also apply the ABCDE rule to your moles yourself to detect changes. If at least one characteristic applies, you should show it to a dermatologist as soon as possible. However, you should consult a dermatologist immediately if the mole
- bleeds or itches,
- becomes larger or
- changes its shape or colour.
Further investigations
If the suspicion of malignant skin cancer is confirmed by the histological examination, further examinations will follow. Imaging techniques are used to check whether metastases have already formed. This includes
- Ultrasound,
- X-ray,
- CT,
- MRI and
- PET.
In addition, a physical examination and, if necessary, the determination of tumour markers in the blood are carried out.
General treatment
Usually no surgery for actinic keratosis
To prevent actinic keratosis from developing into squamous cell carcinoma, it must also be treated. Individual actinic keratoses are often treated by means of cryotherapy. The doctor freezes the skin lesion with the help of a cold spray or in direct contact with the refrigerant for several seconds. This destroys the tissue.
You may feel some local pain during the treatment. Afterwards, the skin area may swell a little and a blister may form. In some cases, scarring or over- or under-pigmentation of the treated area may occur.
If there are several actinic keratoses, the affected skin area can be treated daily for several weeks with a fluorouracil cream. After a phase of inflammation, the actinic keratoses eventually disappear. The tissue is usually not scarred afterwards.
There are also other substances, some of which have to be applied over several months.
Light therapy (photodynamic therapy) can effectively treat actinic keratoses. A cream containing so-called light sensitisers is applied to the skin. These light sensitisers then accumulate in the actinic keratoses. They destroy the tumours under the influence of either daylight or a specific artificial light source.
Surgical removal of actinic keratoses is required,
- if actinic keratoses do not disappear with the help of the methods mentioned,
- if they are particularly raised, or
- if there is a suspicion that they are already growing into neighbouring tissue.
Skin cancer is cut out if possible
Basal cell carcinoma is removed completely by surgery. To be sure that all the cancerous tissue has been removed, the edges of the incision are examined histologically. If the tumour was not completely excised in the healthy tissue, the dermatologist must remove the remaining tumour.
Tumours cannot always be operated on. Sometimes they are in places where they cannot be surgically removed. Some patients are also not fit for surgery. In such cases, under certain circumstances
- radiotherapy or chemotherapy,
- for some tumours also cryotherapy or curettage ("scraping out")
is carried out.
If melanoma is detected at an early stage, the disease can be cured by complete surgical removal of the melanoma in healthy tissue.
If necessary, the wound is covered with a skin graft. If the lymph nodes are already affected, these are also surgically removed.
In the presence of metastases in other organs or in the case of melanomas that cannot be removed,
- Radiotherapy,
- Chemotherapy and/or
- other drug therapies
are used.
Progression and prognosis
Skin cancer is usually curable in its early stages.
Basically, however: The earlier skin cancer is detected, the better the chances of cure. If it is discovered at an early stage, it can be cut out before it can affect surrounding tissue or form metastases.
It is estimated that about five to ten percent of actinic keratoses develop into squamous cell carcinoma. The chances of a basal cell carcinoma being cured are around 95 to 99 percent, while the 5-year survival rate for melanoma is now around 85 percent.
Depending on the type of skin cancer and tumour stage, regular follow-up examinations are recommended. This involves carefully inspecting the area where the tumour was removed, but also all the rest of the skin.
The lymph nodes are palpated, imaging procedures are also used if necessary and tumour markers are determined. In this way, a tumour that may have grown again or appeared elsewhere can be detected and treated at an early stage.
Prevention
Avoid sunburn and excessive sun exposure!
UV radiation is the main risk factor for skin cancer and its precursors. Therefore, it is important that you protect yourself from intense sunlight and prevent sunburn.
Consistently use skin-covering clothing (don't forget your head!) and sunscreen with an adequate sun protection factor on unprotected areas. You should also protect skin areas where actinic keratosis has been treated with a sunscreen.
Sunscreens must be applied sufficiently thickly, evenly and repeatedly (for example after bathing). Note, however, that sunscreens are not suitable for prolonging your stay in the sun – not even with repeated application!

Wearing sunscreen in the sun is a good way to prevent skin cancer © AustrianImages.com | AdobeStock
Your skin can get used to the sun better if you spend regular but short periods in the sun – the skin should not redden. This is especially important in spring and at the beginning of the holiday in regions with higher UV radiation (for example in the mountains or in the "south").
You should use suitable sunglasses if you are in strong sunlight. Also, never look directly at the sun – even if you are wearing sunglasses.
As sunbed users have an increased risk of skin cancer, you should refrain from regular visits to sunbeds. Children and young people are forbidden to visit a tanning salon anyway.
Prevention starts as a child
Also make sure that your children do not get sunburnt. It is best not to expose babies to the sun at all. When the sun is strong, dress your children in clothes that cover the skin not only on the torso but also on the arms and legs.
A cap with a wider brim protects the face and neck and suitable sunglasses protect your child's eyes.











