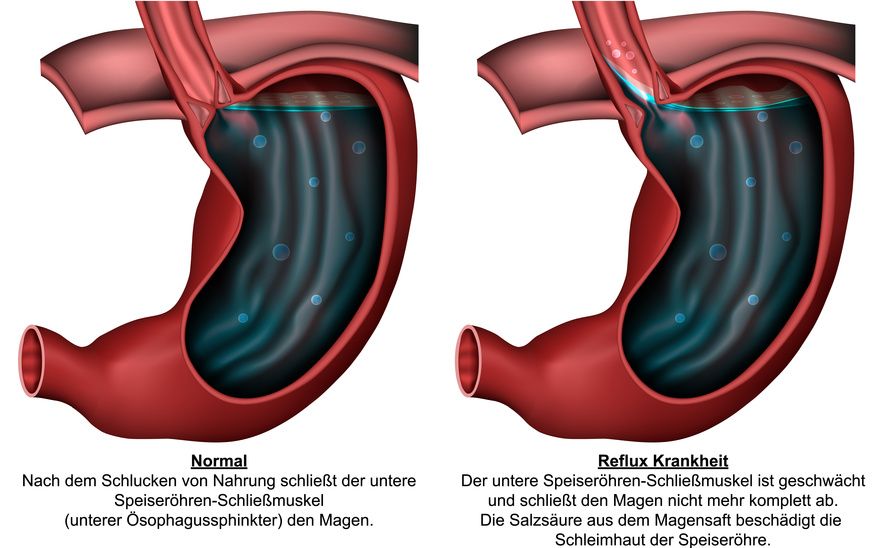
The term reflux disease summarizes various symptoms. What all these symptoms have in common is that they are caused by increased reflux of acidic stomach contents into the esophagus.
This reflux is due to a dysfunctional closing mechanism of the lower esophageal sphincter.
Risk factors that may increase the likelihood of developing reflux include
- Being overweight,
- pregnancy,
- excessive consumption of nicotine and alcohol, and
- various medication.
Two main triggers can be considered as causes of reflux disease:
- The functioning of the lower esophageal sphincter is impaired.
- The motility of the esophagus is reduced.
Both triggers can occur either
- Primarily, without specific reasons, or
- Secondarily, concomitant to other diseases or disorders.
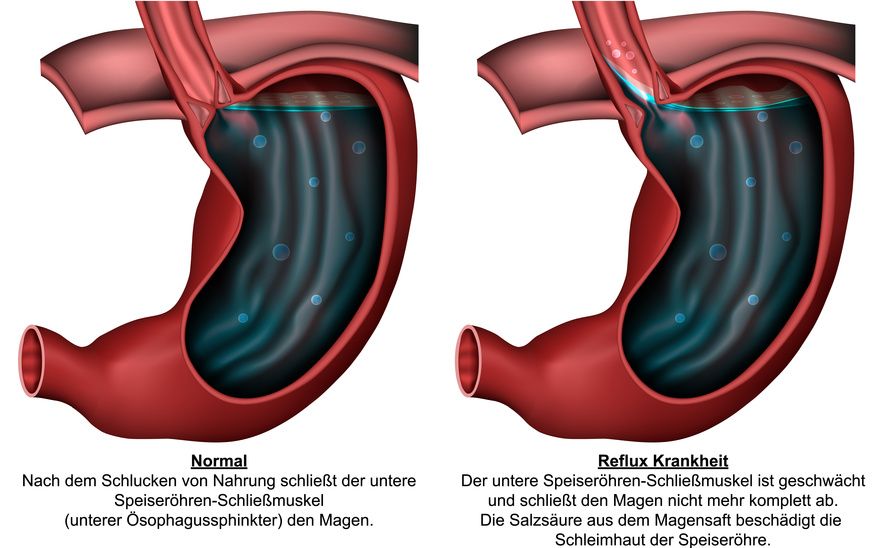
The esophagus and the stomach, healthy on the left, with reflux on the right © bilderzwerg / Fotolia
The leading symptom in reflux disease is usually heartburn. Almost everyone experiences heartburn at least once in their life. It is a burning pain behind the breastbone.
This pain may occur in combination with a sour taste in the mouth as well as frequent belching.
Other symptoms that may be associated with reflux disease include:
- Nausea and vomiting,
- Frequent coughing attacks,
- Inflammation of the larynx and throat area,
- Discomfort when swallowing,
- Pain in the upper abdomen, and
- Frequent hoarseness.
It is characteristic of reflux disease that the aforementioned symptoms often occur
- After a meal,
- After drinking alcohol, or
- After eating sweet or fatty foods.
First of all, during the medical history interview, the physician asks about
- The symptoms of the affected person,
- That person’s general living habits, and
- Any possible comorbidities.
This is followed by a thorough physical exam.
If the suspicion of reflux is corroborated, the physician has various examination options at their disposal.
Endoscopy (esophagoscopy)
An endoscopy is a method of examination used to evaluate the inside of organs. For this purpose, a thin tube called an endoscope is fed through a natural body opening into the affected organ. Via an integrated camera, the image is displayed in real-time and enlarged on a monitor.
In the case of an esophagoscopy, the endoscope is fed through the mouth and throat. It allows assessment of the esophageal mucosa.
The physician can also determine whether and to what extent there is inflammation of the mucosa. It is also possible to collect a mucosal sample during this examination, which is then evaluated in the laboratory with the aim of identifying any tissue changes.
pH-Metry
A pH-metry is another examination option to diagnose reflux. In this procedure, a thin probe is inserted into the patient's esophagus through their nose. It remains there for up to 24 hours.
The aim is to continuously measure the acidity level within the esophagus, i.e., its pH, over a longer period of time.
With the help of this procedure, it can be determined whether and in what quantities stomach contents flow back into the esophagus.
In some cases, an X-ray examination may be useful to accurately assess the swallowing process in the patient. During this procedure, the patient must swallow a contrast medium, which can be seen in the X-ray image.
Some symptoms suggest damage to the respiratory tract. If so, an additional examination by an otolaryngologist also known as an ear, nose, and throat specialist is recommended.
The nutritional factor
In the context of reflux disease, affected individuals often suffer from digestive disorders. These can be curbed with a diet as rich in protein as possible. Proteins stimulate the stomach to produce the hormone gastrin. Gastrin, in turn, improves the muscle tone of the esophageal sphincter so that it can subsequently close again better.
In general, the progression of reflux disease can be positively influenced by a healthy and balanced diet. Small and low-fat and low-carbohydrate portions are recommended.
In addition, it is advisable to eat meals a few hours before going to bed.
Stimulants as a factor
If you have reflux disease, you should completely avoid consuming alcohol if possible. Alcohol causes relaxation of the lower esophageal sphincter and direct damage to the gastric mucosa.
People suffering from reflux disease should generally avoid nicotine. Nicotine leads to an increase in gastric acid production.
However, the influence of coffee on reflux disease is disputed: On the one hand, caffeine can stimulate stomach acid production, which can further irritate the mucous membrane. On the other hand, caffeine increases the production of gastrin, which favors the functionality of the esophageal sphincter.
As a rule, the doctor first prescribes the reflux patient a conventional therapy. The above-mentioned self-help measures may be supplemented by adjunctive medication therapy.
Surgery (anti-reflux plasty) is necessary if
- The symptoms do not improve as a result of other measures or
- The patient does not tolerate the medication well or at all.
Conventional (non-surgical) procedures
In the context of reflux therapy, proton pump inhibitors are the drug of first choice. These drugs are generally shown to be well tolerated. They eliminate symptoms in 70-90 percent of sufferers.
However, once the tablets are no longer taken, half of the patients experience a recurrence of symptoms.
Medications that reduce gastric acidity, so-called antacids, also prove useful.
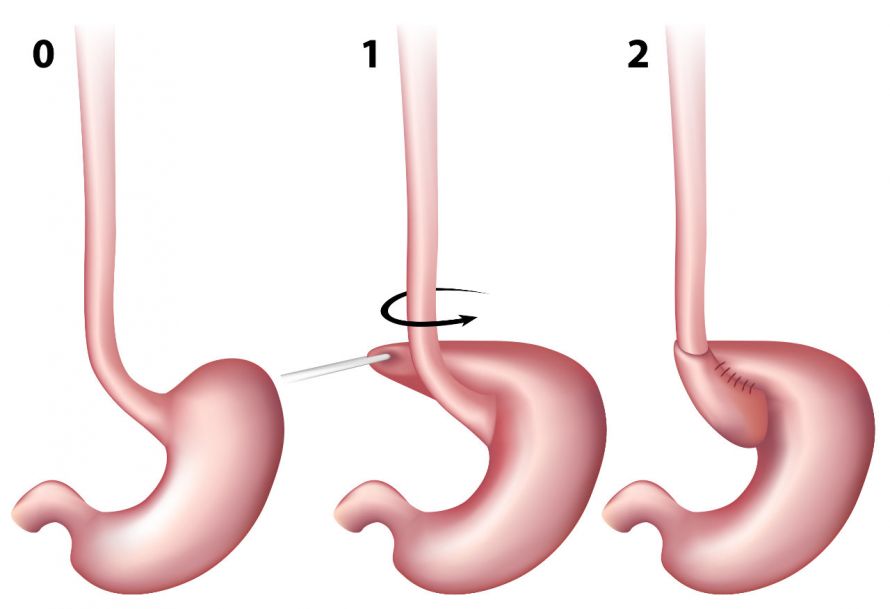
Fundoplication
A fundoplication is a surgical procedure of anti-reflux plasty. It is useful, for example, if reflux disease repeatedly leads to inflammation of the esophagus. Consequently, scarring occurs, which causes the esophagus to narrow.
The goal of fundoplication surgery is to
- Improve the closing function of the lower end of the esophagus sphincter and
- Support the motility of the esophagus.
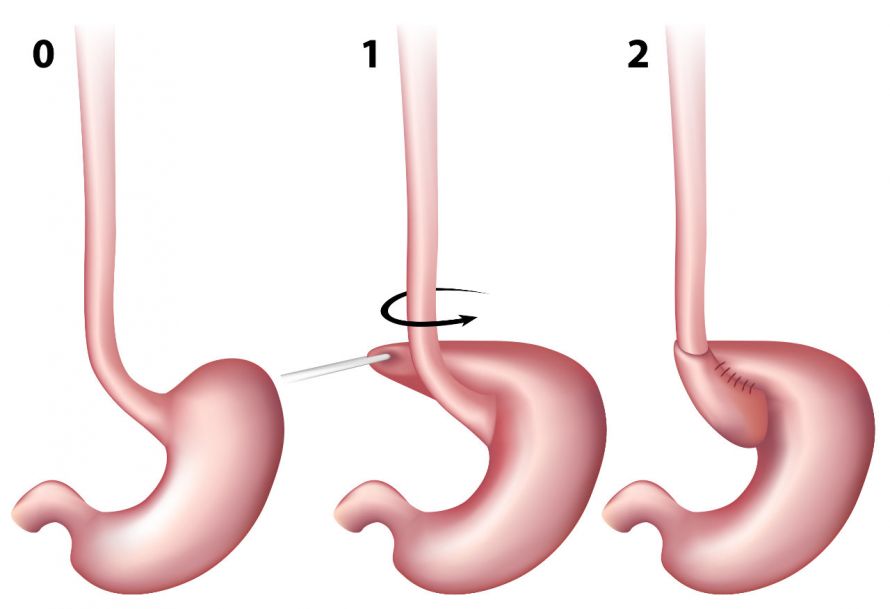
Fundoplication surgery involves placing the upper part of the stomach around the esophageal outlet and suturing it © Alila Medical Media | AdobeStock
Magnetic ring surgery
Magnetic ring surgery is a comparatively new and gentle surgical procedure of anti-reflux plasty. In this procedure, the doctor places a string of magnetic beads around the exit of the esophagus.
The magnetic beads attract each other and seal the anti-reflux valve by pulling the chain together. While swallowing, the beads can separate, allowing food and drink to pass through.
Compared to conventional reflux surgery, the advantages are that
- Vomiting and belching is still possible and
- Bloating and flatulence occur less frequently.
This surgical procedure can usually be performed in a minimally invasive manner. The duration of the operation is about 20 minutes.
Reflux disease symptoms usually lead patients to the family doctor first. In severe cases, internal medicine specialists and gastroenterologists supplement the individual reflux treatment.
These specialists in internal medicine and gastroenterology are specialists in the treatment of reflux disease. After studying human medicine, they specialize in the comprehensive diagnosis and treatment of diseases of the internal organs, in particular the organs of the digestive system, in a residency lasting several years.
Reflux disease is comparatively widespread. It can be successfully treated with the help of self-help measures and, under certain circumstances, adjunctive drug therapy.
Whether surgical therapy is advisable is answered by the specialist after individual consultation and discussion of the findings.