Pancreatic cancer, also known as pancreatic carcinoma, affects about 15,000 people in Germany every year. Mainly older people over the age of 60 are affected. Pancreatic cancer is relatively rare, accounting for about three percent of all cancers in Germany. However, this type of cancer is particularly malignant. It is therefore important to seek treatment from pancreatic cancer experts at specialized centers. Here you can find additional information and selected specialists and centers for the treatment of pancreatic cancer.
Recommended specialists
Brief overview:
- What is pancreatic cancer? Pancreatic cancer is a malignant tumor disease of the pancreas, a hormone-producing gland below the liver.
- Risk factors: Risk factors include smoking and increased alcohol consumption, but also age, genetic predisposition, obesity, and vitamin D deficiency.
- Symptoms: In the early stages, there are no symptoms. Later on, depending on the exact location of the tumor, various symptoms may become apparent, including pain in the upper abdomen, diarrhea, yellowing of the skin, weight loss, and others.
- Diagnosis: If pancreatic cancer is suspected, the first step is usually a transcutaneous ultrasound examination of the abdomen and, if necessary, a CT scan and an MRI.
- Treatment: It can only be cured by pancreatic cancer surgery at an early stage. If necessary, chemotherapy and/or radiotherapy will be administered before or after the procedure. Pain management is also important in palliative care.
- Prognosis: If the disease is detected at an early stage, there is hope for a cure. In later stages, unfortunately, the 5-year survival rate is currently only about 6-7%.
Article overview
Definition: What is pancreatic cancer?
Pancreatic cancer is a malignant tumor disease of the pancreas. It is also called pancreatic carcinoma.
The pancreas is located in the upper abdomen and produces digestive enzymes, which it releases into the duodenum. It is also involved in regulating blood sugar and releasing hormones into the bloodstream.
In principle, the tumor can develop in any part of this elongated organ, but the head of the gland is affected most often.
Most pancreatic cancers arise in the exocrine region, the part of the pancreas that secretes digestive enzymes. Therefore, this carcinoma is also called pancreatic exocrine cancer (mostly ductal adenocarcinoma).
If a malignant tumor develops in the endocrine part responsible for blood glucose regulation, the patient has a pancreatic endocrine tumor, which differs in behavior from an endocrine tumor.
Pancreatic carcinomas metastasize frequently and relatively quickly.
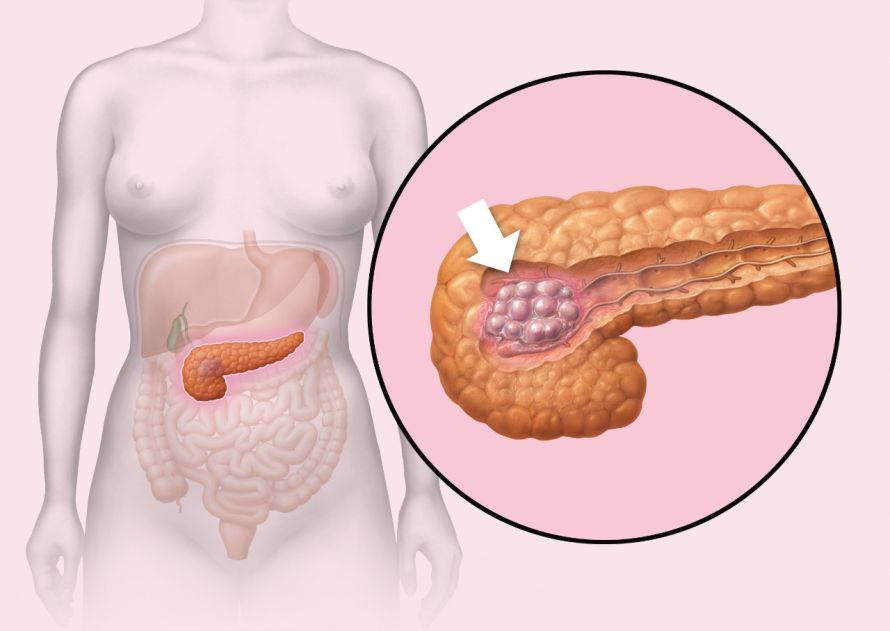
The location of the pancreas and a depicted tumor in the head of the pancreas © lom123 | AdobeStock
Causes and risk factors for pancreatic cancer
The exact causes of the development of pancreatic cancer are not yet known. However, there are factors that are known to increase the risk of disease. Risk factors include smoking and increased alcohol consumption.
In addition, old age and a genetic predisposition play an important role.
Diabetes and a hereditary type of chronic pancreatitis also appear to slightly increase the risk.
Other risk factors can be found in one’s personal lifestyle:
- Being severely overweight,
- A high-fat diet, and
- Vitamin D deficiency.
Symptoms of pancreatic cancer
In pancreatic cancer, early symptoms are largely absent, so the tumor is often discovered late.
Symptoms only become noticeable when the tumor disease is already advanced. Thus, depending on the location of the tumor,
- Pain in the upper abdomen that may radiate to the back,
- Diarrhea,
- Fatty stools (steatorrhea),
- Yellowing of the skin,
- Weight loss,
- Bloating, and
- A deterioration of one’s general condition,
among other things, may occur. If metastases have formed, further organ-specific symptoms occur, such as pressure pain in the liver.
From training.seer.cancer.gov; original SVG: Cradel - translation of File:Illu pancrease.svg; http://training.seer.cancer.gov/module_anatomy/images/illu_pancrease.jpg, in the public domain, Link
Diagnosing pancreatic cancer
Some laboratory values are elevated in tumor-related jaundice. These include
- Gamma-glutamyltransferase,
- Alkaline phosphatase, and
- Direct bilirubin.
However, there is no specific laboratory test to diagnose pancreatic cancer. If pancreatic cancer is suspected, the first step is usually a transcutaneous ultrasound examination of the abdominal cavity. Because the conclusiveness of this sonography depends on the examiner, it should be performed by an experienced pancreatic cancer specialist.
Endoscopic ultrasound examinations are more high-resolution, enabling even smaller tumors to be detected.
The standard procedure for preoperative diagnosis is contrast-enhanced thin-slice computed tomography (CT scan). Magnetic resonance imaging (MRI) can also be used for better visualization of the soft tissues.

An MRI is a good way to visualize the soft tissues and thus find indications about the spread of the tumor or its metastases © Nejron Photo | AdobeStock
Treating pancreatic cancer
A cure for the tumor disease can only be achieved by early surgical removal of the carcinoma. To ensure that all cancer cells are killed, this is often followed by subsequent (adjuvant) chemotherapy.
However, the majority of tumors are discovered at a late stage, when no cure by surgery is possible. However, there are initial studies in which an inoperable tumor was reduced in size to the point where surgery could be performed. These included treatment with neoadjuvant (preceding surgery) chemotherapy and/or radiotherapy.
Otherwise, radiotherapy does not play a major role in pancreatic cancer therapy.
Chemotherapy is not only used in adjuvant therapy (i.e., after a pancreatic cancer surgery) but also in the palliative situation. Palliative care aims to control tumor growth and symptoms associated with the tumor. This is intended to improve the quality of life and prolong it. However, a cure is no longer possible.
Even pain management is significant in pancreatic cancer. An appropriate, highly dosed administration of pain medication allows the patient to participate in social and community life.
Which specialists and specialty clinics treat pancreatic cancer?
Patients with pancreatic cancer should seek treatment at specialized pancreatic cancer clinics that have a lot of experience with pancreatic cancer. There, high-quality treatment can be guaranteed and, where appropriate, patients can benefit from the latest therapies by participating in clinical trials.
The German Cancer Society (DKG) certifies such interdisciplinary oncological treatment centers as pancreatic cancer centers, which ensures high-quality care for patients with pancreatic cancer according to the most state-of-the-art and modern treatment options (guidelines).
At these facilities, there are so-called tumor conferences in which various pancreatic cancer experts work together in an interdisciplinary manner. They take into account the diagnostic and therapeutic procedures recommended by guidelines in order to create a customized treatment concept for the individual patient. As a rule, these are specialists from the following fields
- Gastroenterology,
- Oncology,
- Radiotherapy,
- Radiology,
- Surgery, and
- Pathology.
The German Society for General and Visceral Surgery (DGAV) carries out equivalent certification for centers dedicated to surgical pancreatic diseases including pancreatic cancer. Here, too, external experts regularly review compliance with guidelines and especially monitor the quality of treatment.
Prognosis for pancreatic cancer
The prognosis depends primarily on the stage at which the pancreatic cancer was discovered. In early stages, there is a chance of being cured.
In later stages, treatment is primarily palliative, because then the prognosis is very unfavorable. Thus, the 5-year survival rate is only 6 to 7%.
However, with new therapeutic concepts, there is hope that treatment outcomes will improve in the future.