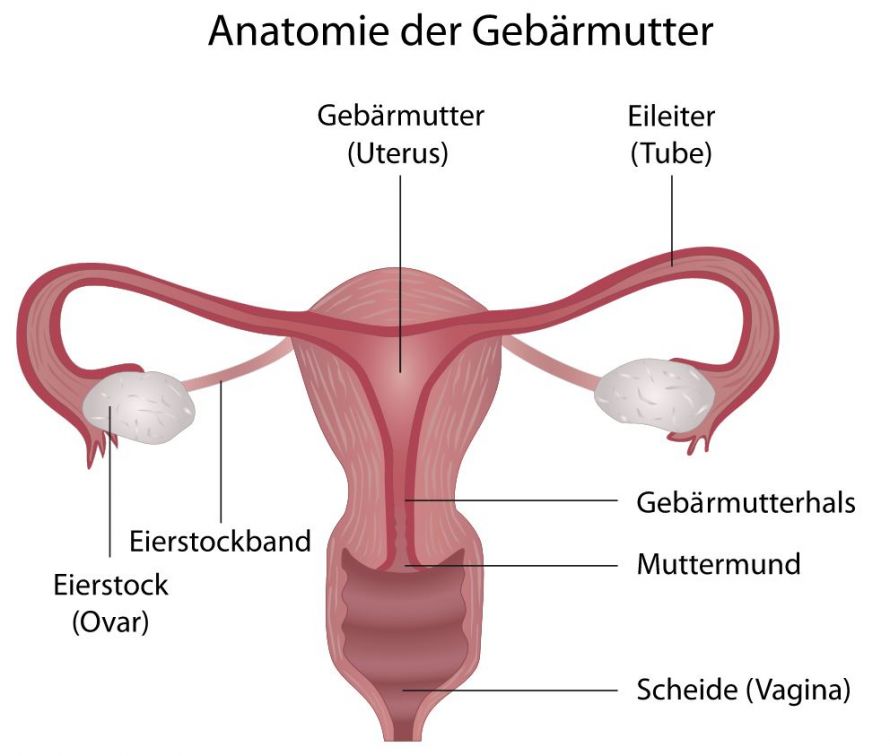
Cervical cancer is a malignant change in the cervical tissue. The cervix is located in the lower part of the uterus. In technical language, the cancer is also called cervical carcinoma.
Cervical cancer has nothing to do with uterine cancer (cancer of the uterus) and should not be confused with it!
Statistically, women between the ages of 40 and 59 are particularly likely to be affected by cervical cancer. Many women are even younger when diagnosed.
In the early stages, cervical cancer often goes unnoticed. In the advanced course of the disease, it can lead, among other things, to
- Spotting,
- Pain, and
- Vaginal discharge.
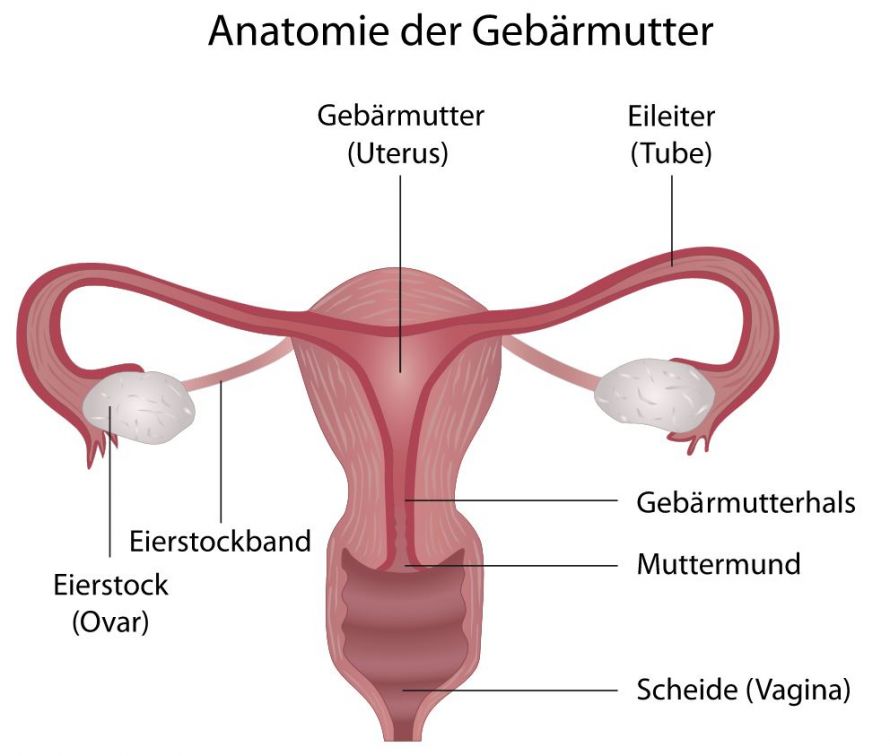
Cervical cancer develops in the cervix, the lower part of the uterus © bilderzwerg | AdobeStock
In most cases, the cause of cervical cancer is human papillomavirus (HPV) infection. Some of these types of viruses are particularly aggressive and trigger tissue changes that lead to this type of cancer.
HPV are transmitted during sexual intercourse. Normally, the immune system successfully fights them off. Nevertheless, some viruses may remain in the uterine lining. There they can then cause tissue changes over time.
In simple terms, it can be stated that cervical cancer is the direct result of an infection. There is a vaccine that protects against this infection, the so-called HPV vaccine. The patient must be vaccinated before their first sexual intercourse.
Most often, cervical cancer does not cause any symptoms in the early stages. The affected woman therefore does not notice the underlying infection.
As the disease progresses, the following symptoms may appear, e.g.:
- Intermittent bleeding outside the normal cycle,
- Bleeding after sexual intercourse,
- A strong-smelling discharge, and
- Pain during sexual intercourse as well as in the pelvic area.
Further discomfort does not necessarily occur directly in the lower abdomen. Uterine cancer can be indicated by
- Back pain,
- Weight loss,
- Swelling, and
- Urinary tract infections.
Since the disease shows no symptoms for quite some time, early screening from the age of 20 is recommended. From this age on, health insurance companies pay for an annual check-up.
These examinations are also necessary for women who have been vaccinated against the HPV virus. Vaccination does not guarantee one hundred percent protection.
During the examination, the doctor examines the cervix and takes a sample from the cervical canal. These samples are then examined in more detail as part of a Pap smear. The laboratory looks for cell changes that may indicate a possible disease.
The period between medical examinations depends on the type of change. A colonoscopy or a biopsy may also be used as part of the medical examination.
The type of therapy depends on the stage of the disease.
Precancerous lesions can be completely removed with cervical conization. In the very early stages of this invasive cancer, conization may also be sufficient.
It is often necessary to remove the uterus if the cervical cancer is more advanced. This requires a radical hysterectomy, i.e., the surgeons also remove the entire supporting apparatus of the uterus. The lymph nodes in the lesser pelvis and along the abdominal aorta can be affected by cancer cells and are also removed.
After the surgery, the doctors decide whether further radiotherapy in combination with chemotherapy is necessary.
If the tumor cannot be removed surgically, a combination of radiotherapy and chemotherapy may also be the only possible treatment.
In the early stages, the chances of curing cervical cancer are considered very good. This is true for both precancerous and early cancer stages.
However, if the tumors grow or spread to other areas of the body, the chances of curing the cancer decrease.
Preventing cervical cancer means preventing the preceding HPV infection.
Girls should definitely be vaccinated against HPV. Vaccination does not provide complete protection but significantly reduces the risk of infection. Since HPV are transmitted via sexual intercourse, patients should be vaccinated at a young age.
Practicing safe sex can also help. While condoms cannot eliminate all dangers of virus transmission, they do reduce the risk.
Otherwise, you should always take advantage of annual cancer screenings, even at a young age. In this way, dangers can be detected and treated at an early stage.