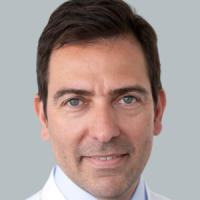
Thyroid cancer is a rare and malignant form of cancer that originates from degenerated thyroid cells. However, not every change is the thyroid is malignant cancer. Most enlarged thyroids are caused from iodine deficiencies. Hyperthyroidism, hypothyroidism, or benign cysts can also lead to an enlarged thyroid (goiter, struma). Only in rare cases will it actually be thyroid cancer, which is also referred to by doctors as thyroid carcinoma or struma maligna (malignant goiter).
Thyroid cancer can cause the thyroid gland to become enlarged © amazing studio | AdobeStock
Physicians differentiate between four different types of thyroid cancer depending on which tissues are tumorous. They are also different in regards to their aggressiveness, progression, and prognosis:
- Papillary thyroid carcinoma is the most common malignant thyroid tumor, and it occurs most frequently in people between 40 and 50 years old. The chance of recovery is very good. These tumors sometimes grow not only one node, but rather numerous tumorous lesions in the thyroid. The metastasis of cancer cells happens primarily over the lymph vessels.
- Follicular thyroid carcinoma, that comes from follicle cells, appears most often in people between 50 and 60 years of age. It is likewise easily treatable. The tumor most often is only a single node.
- Anaplastic thyroid carcinoma is uncommon, usually appears in those over the age of 60, and grows rapidly and can metastasize quickly.
- Medullary thyroid carcinoma (C-cell-carcinoma), which comes from the calcitonin-producing C-cells, is also very uncommon. Although it grows slowly, it affects the lymph nodes of the throat early and also affects other organs later on.
Papillary thyroid cancer is the most common form © bilderzwerg | AdobeStock
Thyroid cancer is one of the rarest types of malignant cancer. Thyroid cancer is the 15th most common form of cancer in men, and the 14th most common in women. The average age of patients diagnosed with it is 55 years old, but women are more than twice as likely as men to be diagnosed with thyroid cancer. In Germany, between 5,000 and 6,000 people develop thyroid cancer per year. Some 700 to 800 people die from it. This means that 0.2 to 0.3 percent of all cancer deaths are caused by thyroid cancer. Rates of thyroid cancer are rising in all age groups worldwide.
Thyroid carcinoma is the consequence of degenerated thyroid cells. The cells that can degenerate into thyroid cancer include
- Cells that create thyroid hormones, and
- So-called C-cells, that surround the thyroid hormone-producing cell groups and produce the hormone calcitonin.
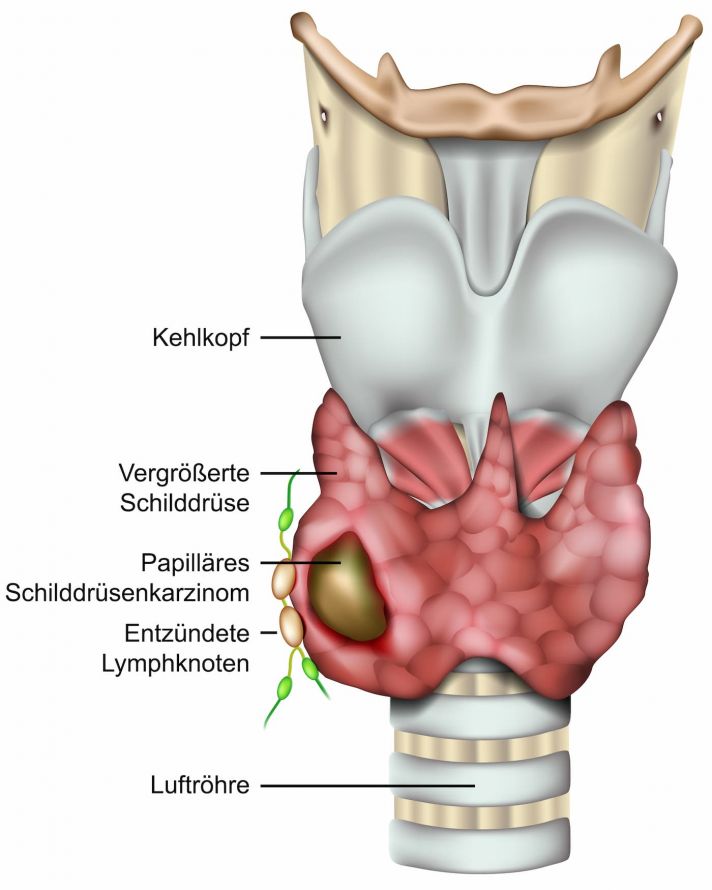
The tissue type is of great importance to the treatment and prognosis of thyroid cancer. Nodular thyroid changes require special attention. In scintigraphic diagnostics, they appear as “cool or cold nodules” (low-functioning or dysfunctional thyroid tissue) and are often associated with thyroid cancer. An ultrasound examination shows that the nodules, which have an increased risk potential, often appear less echogenic.
A closer examination is necessary in the case of so-called “cold nodules” © bilderzwerg | AdobeStock
Thyroid cancer can grow into surrounding tissues, much like any malignant tumor. Furthermore, additional tumors can form (metastases). They develop from the spread of tumor cells through the lymph vessels into the surrounding lymph nodes and also into the lungs (lung metastases) and bones through the bloodstream.
Medullary thyroid carcinoma can occur in a familial manner in 1/4 to 1/3 of cases and it can also be associated with the growth of new tumors in the adrenal medulla and the parathyroid glands.
The causes of thyroid cancer are not yet fully understood. Because thyroid carcinoma appears more frequently in some families, thyroid specialists assume that there is a genetic predisposition, especially for the medullary type.
Another risk factor is high-energy radiation, like the radiation that occurs during x-ray examinations. For instance, x-ray irradiation of the neck area during childhood is particularly problematic. After the Chernobl reactor disaster, scientists in the areas that were particularly affected found a connection between the intensity of the radiation and the frequency of thyroid cancer in children.
An enlarged thyroid (struma, also called a goiter) alone is not considered a risk factor for the development of cancer. Special medical attention is only required in the event of certain changes to the tissues or the formation of lumps.
In its early stages, there are usually no symptoms of thyroid cancer. If an enlargement of the thyroid gland (struma, goiter) develops within a few weeks and feels very coarse, an immediate visit to a doctor is recommended. The same applies if a long-standing goiter suddenly continues to grow. An increase in the circumference of the neck can be found by taking a measurement. It is usually noticeable when the top button on a shirt or blouse can no longer be buttoned. Tough, palpable lumps in the neck area are also a possible symptom. These may be enlarged lymph nodes.
An enlarged thyroid and palpable lumps are possible symptoms of thyroid cancer © medistock | AdobeStock
In most cases, a doctor’s evaluation is necessary to differentiate between a benign goiter and malignant thyroid cancer. Some complaints may be explained by the location of the pathologically altered thyroid gland on the windpipe and its proximity to the larynx, esophagus, and the vocal cord nerve that runs behind the thyroid gland. A feeling of pressure in the throat, difficulty swallowing, shortness of breath, or an urge to cough do not necessarily indicate a malignant disease. If you experience sudden hoarseness, you should see a doctor at once to identify the cause of this symptom.
As with any kind of cancer, early diagnosis and treatment of thyroid cancer is important and an essential requirement for a good chance of recovery. Firstly, the doctor will evaluate your medical history as part of an anamnesis interview. Your description of your symptoms and their duration are important to doctors. Information about cancer within your family or possible exposure to ionising radiation in childhood and adolescence is also very useful. Examination methods used to diagnose thyroid cancer include:
- Palpation examination of the throat
- Ultrasound examination of the thyroid
- Scintigraphy of the thyroid
- Laboratory tests
- Imaging examination procedures (x-ray, CT, MRI)
- Fine needle biopsy
- Genetic analysis
Palpation Examination of the Throat
The doctor will palpate the thyroid gland with the fingers of both hands. In this way, they first obtain information about the size and surface of the organ. It is important to check the ability of the thyroid to swallow and also to determine whether the lumps feel particularly coarse. The doctor will also scan the throat area for noticeable, palpable lymph nodes.
Ultrasound Examination of the Thyroid
If a tumor is suspected after the palpation of the thyroid, the next step is to perform an ultrasound examination of the thyroid gland. The ultrasound provides information on the location, size, and boundaries of the thyroid gland and perhaps any lumps in the thyroid gland. Because tissue changes reflect the ultrasound signal differently, the labels “hypoechoic” or “hyperechoic” can be used to make initial claims about pathological changes. A definitive clarification of the benign or malignant nature of the nodules is not yet possible with this method.
Examination of the thyroid glands by means of ultrasound © Alexander Raths | AdobeStock
Scintigraphy of the Thyroid
Thyroid scintigraphy can be used to distinguish between hot and cold nodules. For this purpose, the doctor administers a weak radioactive substance (technetium). This accumulates in the thyroid tissue and provides information on metabolic activity. Nodular areas with reduced or no metabolic activity are “cold nodules” and require special checks and evaluations. An additional special scintigraphy (MiBi) can also help to better classify the suspicious areas.
Laboratory Tests
A blood test for thyroid hormones, especially for triiodothyronine (T3) and tetraiodothyronine/ thyroxine (T4), gives the first indications of a thyroid disease and evidence about the activity of the thyroid gland.
A tumor marker (calcitonin) is available for only one type of thyroid carcinoma, which enables early detection of this type of tumor. If needed, this is followed by a special test to check this value. However, most types of thyroid cancer cannot be determined by laboratory tests.
Thyroid gland palpation and blood tests for thyroid hormones © Peakstock | AdobeStock
Imaging Examination Procedures
With the help of imaging procedures, doctors can obtain additional information about the carcinoma if needed:
- An x-ray of the trachea or esophagus provides information about the narrowing of these structures by the tumor.
- An x-ray of the chest provides information about the growth of the thyroid in upper chest area. It is also used to look for any metastases in the lungs when tumors are detected.
- With special examinations like computer tomography and magnetic resonance tomography, doctors receive detailed information about the growth in surrounding structures in the case of large tumors. This is important when choosing the appropriate therapy.
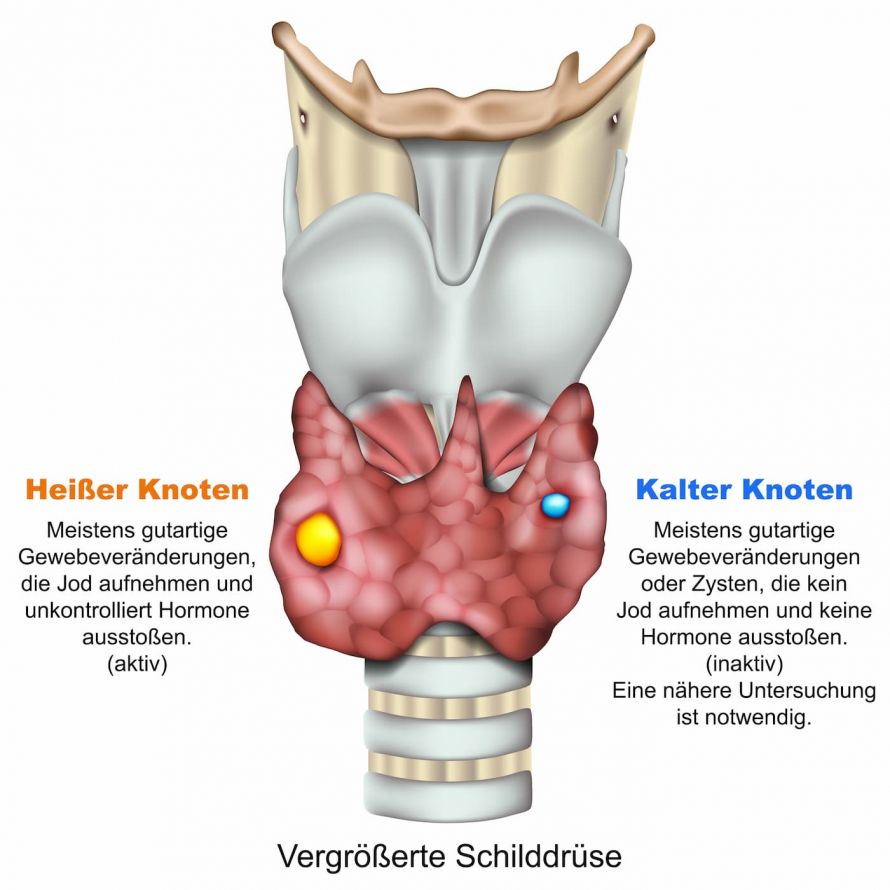
Fine Needle Biopsy
A fine needle biopsy is used to test tissues for malignant tumor cells. A doctor will puncture a “cold nodule” under ultrasound to obtain cells for microscopic examination. In some cases, a biopsy can be used to determine the type of thyroid cancer before an operation. This method has its limits, however, so not every examination can detect thyroid cancer or rule it out with certainty. In these cases, the final histological examination takes place after the thyroid gland has been surgically removed.
A fine needle biopsy of the thyroid is used to obtain a tissue sample for microscopic examination © bilderzwerg | AdobeStock
Genetics
Concerning medullary thyroid carcinoma, a genetic analysis (to detect the RET proto-oncogene mutation) can provide possible evidence for familial clustering and the need to examine family members. This analysis also provides information on the connection between this special thyroid cancer and other diseases such as tumors of the adrenal medulla or parathyroid gland.
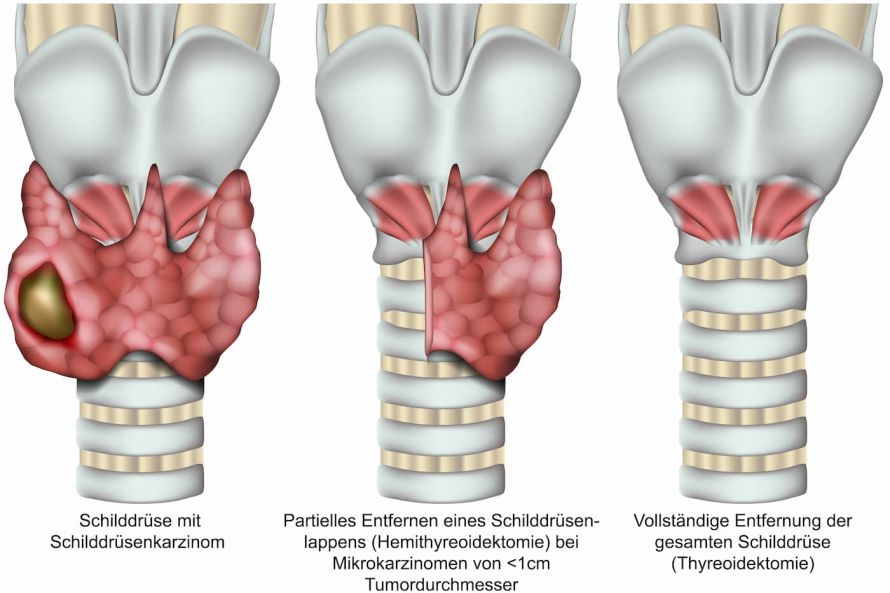
There are several different therapies that can be used to treat thyroid cancer. The most important treatment option for thyroid cancer is the surgical removal of the thyroid (thyroidectomy). As part of this thyroid operation, the surgeon usually also removes the lymph nodes of the neck.
Surgery involves the partial or complete removal of the thyroid © Bergringfoto | AdobeStock
If the histological examination of the removed tissue confirms a malignant tumor, radioiodine therapy may follow a few weeks later. Radioactive iodine accumulates in any remaining thyroid tissue, causing it to die. This treatment method is the most common form of therapy for thyroid gland carcinoma and is very effective.
Since removing the thyroid means the body will lack important hormones, the patient must begin medicinal hormone therapy. Hormones supplied by the thyroid, such as L-Thyroxin, are replaced by this hormone therapy.
Radiation treatment for thyroid cancer is an option if there are still remnants of tumor tissue in the body that cannot be treated with surgery or radioiodine therapy.
Thyroid cancer is usually not susceptible to chemotherapy. Therefore, chemotherapy can only be considered for the advanced stage of thyroid cancer when metastases are already present.
Deciding which type of therapy to use to treat thyroid cancer depends entirely on which type of thyroid cancer it is.
Papillary Thyroid Carcinoma
This is the most common form of thyroid cancer, in which one or more tumors can be detected in the thyroid gland. If the tumor metastasizes, this takes place through the lymph vessels into the surrounding lymph nodes. Papillary thyroid carcinoma has the best chance of recovery (ten-year-survival rate is about 93 percent).
Based on knowledge of tumor biology, this type of cancer does not require the complete removal of the thyroid gland or the lymph nodes for a single small tumor (up to 1cm in size, called a microcarcinoma).
The partial or complete removal of the thyroid © bilderzwerg | AdobeStock
For larger tumors or evidence of multiple tumors, the treatment consists of
- surgically removing the entire thyroid and the removal of the cervical lymph nodes between the two oblique cervical muscles and
- subsequent radioiodine therapy.
If the result is an incidental finding after a normal thyroid operation, the follow-up operation will take place as soon as possible.
Follicular Thyroid Carcinoma
This type of thyroid cancer is likewise common. It also has very good rates of recovery (the ten-year-survival rate is around 85 percent). However, this depends on a further division into special subgroups of this type of thyroid cancer. Cancer metastases preferentially occur via the bloodstream into the lungs and bones, but lymph nodes can also be affected.
According to recent findings, even with this type of cancer in a certain subgroup, if a “microcarcinoma” is found, no extensive removal of the thyroid gland or lymph nodes is required. Standard therapy for all other tumors is also used for this type, like
- completely removing the thyroid gland and the surrounding cervical lymph nodes as well as
- subsequent radioiodine therapy.
Anaplastic Thyroid Carcinoma
This rare type of thyroid cancer is quite malignant and occurs more commonly in older patients. Because of rapidly-growing tumors in the surrounding area and the metastases, curative surgical treatments are not always possible. Radiation therapy is used to avoid complications from the carcinoma.
Medullary Thyroid Carcinoma
This form of thyroid cancer is rare. It is the only form of cancer for which a tumor marker (calcitonin) is available, which can be determined by taking a blood sample. Because this type of cancer develops from C-cells, radioiodine therapy is impossible due to a lack of iodine storage. Therefore, surgery is the method of choice.
In addition to the complete removal of the thyroid gland, extensive removal of cervical lymph nodes and in some cases the lymph nodes in the chest area is also necessary because of premature lymph node tumors. Surrounding organs are only removed in the case of advanced tumors.
The average ten-year survival rate is 75 percent. The decisive factors for this prognosis are the spread of the tumor beyond the thyroid gland and the detection or absence of metastases.
Genetic analysis is required for this form of thyroid cancer. It serves to clarify to what extent there is a familial link or the relationship to other diseases. Affected family members are treated using an individualized therapy concept. This depends on the specifically determined genetic change.
The course and prospects for recovery from thyroid cancer depend primarily on the type and the initial spread of the thyroid cancer. In addition, this general rule in cancer treatment applies: the earlier that cancer is diagnosed and treated, the better the chances of remission. The involvement of the lymph nodes seems to have only a minor influence on the prognosis.
With the most common forms of thyroid cancer (papillary and follicular carcinoma), the chances of recovery are usually very good after the treatment methods of surgery and radioiodine therapy have been carried out. Because papillary carcinoma and follicular carcinoma rarely metastasize, patients with these types of cancer can completely recover in 80 to 90 percent of cases.
If medullary carcinoma is detected early, the chances of recovery are similar; with metastases, the 5-year survival rate is 50 to 60 percent.
The recovery and prognosis are difficult to predict in rapidly and very aggressively growing anaplastic thyroid carcinomas. In this type of cancer, the 5-year survival rate is less than 10 percent.
A thyroid specialist is a specialist in oncology who plans and carries out treatment in an interdisciplinary team with specialists from other fields (like endocrine surgery and nuclear medicine). Patients should seek treatment in specialized clinics for thyroid cancer, where high quality treatment is guaranteed. In addition, patients may also benefit from the latest therapies by participating in clinical trials.