Recommended specialists
Article overview
Vascular surgery - Further information
Vascular surgery is regarded as a separate surgical specialism. Although influenced by developments in general surgery and cardiac procedures, as well as the more-recent minimally invasive procedures, vascular surgery is principally concerned with diseases of the vascular system, i.e. arteries, veins and lymphatic circulation. These are often managed by a range of medical therapies and minimally invasive catheter procedures, as well as via surgical reconstruction.
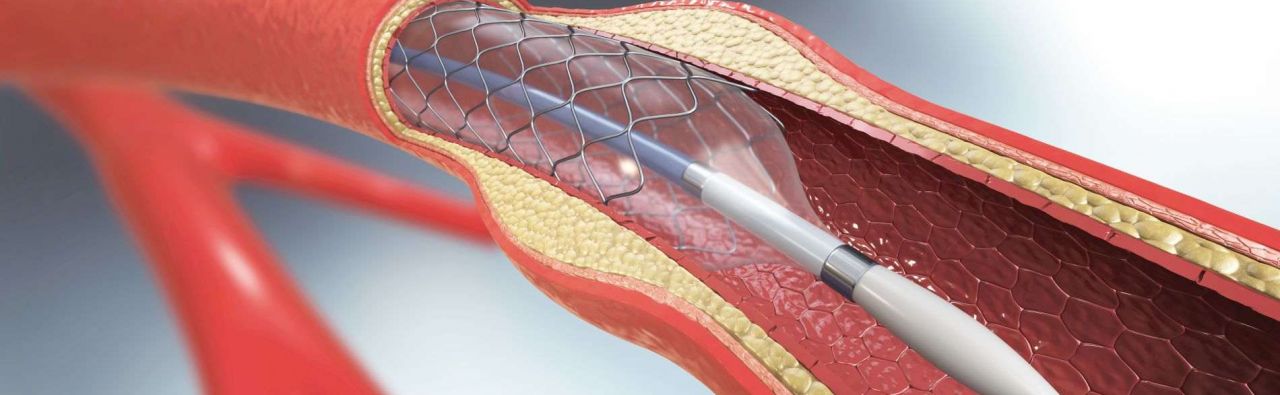
The therapeutic range of services in vascular surgery comprises, in particular, endoscopic aortic surgery, endovascular aortic surgery, minimally invasive surgery, angioplasties (vascular dilatation using balloon catheter) PTA, stent implantations (insertion of vascular supports), endografts (placement of vascular prostheses via catheter systems), laser surgery, the treatment of peripheral vascular occlusive disease, the CHIVA method and the application of Cava filters.
Specialists for vascular surgery
A vascular surgeon is a specialised physician who focuses on the operative and medical treatment of diseases of the arteries and the veins with the associated consequential damage. Scraping out and widening blood vessels, placing a bypass and dilating vessels in case of arterial occlusion and circulatory disorders or placing a prosthesis to widen arteries are all medical focal points of the qualified vascular surgeon. The reconstruction of the arteries of the neck, varicose veins, deep vein thrombosis and diabetic foot, CVA prophylaxis with arteriosclerosis, arterial occlusion disease and aneurysms of the aorta of the abdomen, neck and pelvis are the most frequent indications for vascular surgical procedures.
In addition to specialised operative skills, vascular surgeons possess knowledge concerning diagnostic procedures as well as disease-related preoperative and postoperative care. To become a specialist in vascular surgery, a physician must complete six years of postgraduate training.
What does vascular surgery help with?
Traditional open vascular surgery is used to relieve a broad range of conditions. Meanwhile, the gradual evolution of endovascular surgical procedures has developed additional techniques and further extended the range of vascular surgical interventions. Where an endovascular surgery option is available for your condition, it is often a less invasive and perhaps a lower-risk alternative (though there is always a range of factors to consider). Endovascular surgery typically involves making a small incision on each side of your hip area in order to gain internal access to blood vessels.
Vascular surgery may be recommended to help with:
- Open or endovascular repair of abdominal aortic aneurysms (swellings), thoracic aortic aneurysms and thoracoabdominal aneurysms, including fenestrated and branched stent grafts (a stent is a small mesh tube)
- Open or endovascular surgical reconstructions and balloon angioplasty (repair or unblocking of a blood vessel) and stenting (inserting of mesh supports) in all vascular regions
- Carotid endarterectomy (unblocking of a carotid artery) and carotid artery stenting
- Bypass surgery and endovascular therapy for PAD (peripheral artery disease) and gangrene of the limbs
- Open and endovascular surgical treatments for peripheral artery aneurysms
- Endovenous laser therapy treatment, subfascial endoscopic perforator surgery or radio-frequency ablation for varicose veins and venous ulcers
- Endovascular and open surgical reconstruction for deep vein occlusions (blockage or closure of a vein)
- Hemodialysis access (using a surgically created vein for vascular access)
- Treatment of vascular malformations, MALS (median arcuate ligament syndrome, which involves compression of the celiac artery), nutcracker syndrome (a vascular compression disorder), lymphedema (swelling within the lymph system), and chylous effusions (fluid gathering in the chest)
When is vascular surgery used?
The primary aim of vascular surgery is to resolve problems within the vascular system (bodily veins and arteries), such as venous ulcers or varicose veins. Modern surgery tends to use minimally invasive peripheral arterial interventions whenever possible in order to offer a more rapid recovery.
What are the risks of vascular surgery?
Some risks are generally attached to all kinds of surgery. For instance, surgical incisions carry a risk of infection around the area of the wound. In addition, operations in the chest region, or those procedures that involve major arteries and blood vessels, will usually involve a higher risk of surgical complications. Furthermore, patients whose lifestyle choices include smoking, or who may have hypertension (high blood pressure), chronic kidney or lung disease, or many similar illnesses, are also at greater risk of further complications, both during and after surgical procedures. Other possible risks of vascular surgery may include:
- bleeding
- failed or blocked grafts
- stroke or heart attack
- possible leg swelling if a vein is taken from the leg
- for those over 65 years of age, there is an increased risk of brain impairment following major vascular surgery, and the more damage that has occurred to the circulatory system prior to any surgical intervention, the greater the chance that some kind of mental decline may be experienced after vascular surgery
- impotence
The best course of action is always to discuss the possible risks with your doctor and the vascular surgeon once they have conducted a thorough physical examination and carefully reviewed your previous medical history.
Are there alternatives to vascular surgery?
Although this is not an area where extensive research has been carried out, there seem to be few alternatives to vascular-type diseases that do not involve vascular surgery. Acupuncture is quite often used to reduce the symptoms of hypertension, and chelation therapy – a chemical treatment used to rid the body of minerals and/or heavy metals – is claimed to stabilise the effects of vascular disease, though its effectiveness is currently unproven. Health-wise, the priority should be maintaining a sensible diet and taking note of any previous family history of vascular disease in order to recognise and address the symptoms as early as possible.
Medical spectrum
Therapies
- (Vein) Stripping
- Abdominal aortic aneurysm surgery
- Aneurysm surgery
- Aortic stent
- Aortic surgery
- Aortic valve reconstruction
- Balloon catheter dilatation PTCA
- Carotid artery PTA
- Dialysis shunt insertion
- Endovascular treatment
- Enucleation surgery
- Shunt
- Stent implantation
- Thrombectomy
- Vascular surgery
- Vein sclerotherapy