Unlike ventricular fibrillation, atrial fibrillation is not life-threatening. However, those affected have an increased risk of having a stroke or heart attack or suffering from heart failure. Untreated, prolonged atrial fibrillation often causes an increase in the size of the heart atria.
The earlier the heart disease is detected and treated, the sooner the patient can regain their normal sinus rhythm.
Paroxysmal (seizure-like) atrial fibrillation is often asymptomatic. Some sufferers only notice a slight drop in performance. Other patients with cardiac arrhythmias have the following symptoms:
The symptoms that occur depend on whether the heart is
- too fast,
- rather normal or
- too slow
pumps irregularly.
Rapid beats are felt as a frightening racing of the heart, often accompanied by shortness of breath and severe chest pain.
With normal speed, fatigue often occurs.
Slow cardiac arrhythmias usually lead to dizziness. In the worst case, the affected person may faint.
Chronic atrial fibrillation is rarely noticed by the patient because the heart muscle has already become accustomed to the irregular pumping.
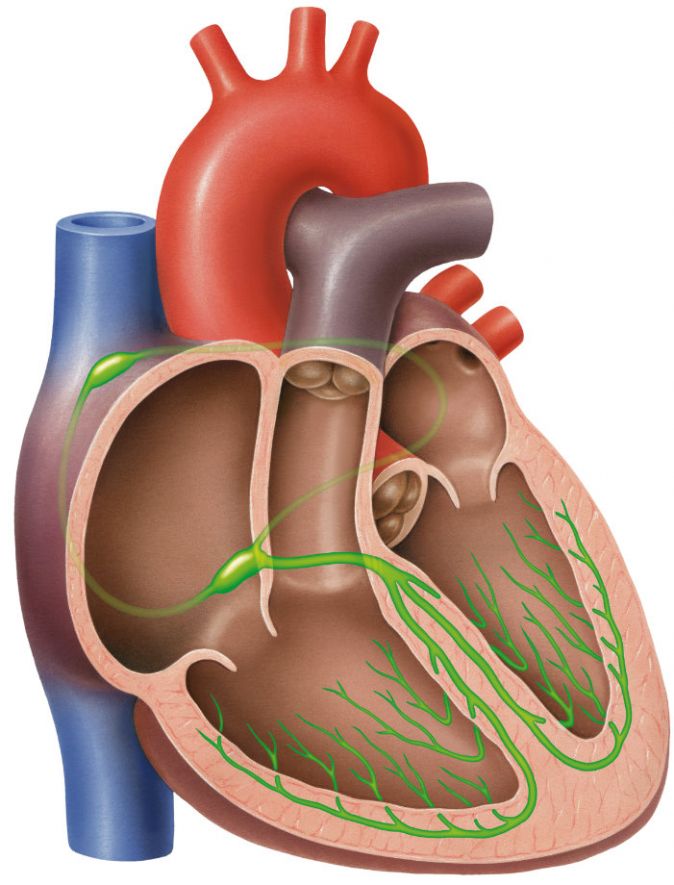
In healthy people, the sinus node in the right atrium sends out an electrical impulse that is transmitted to the ventricles. There it causes the heart muscle to contract. This is how the heartbeat is created. This pumps the blood into the body.
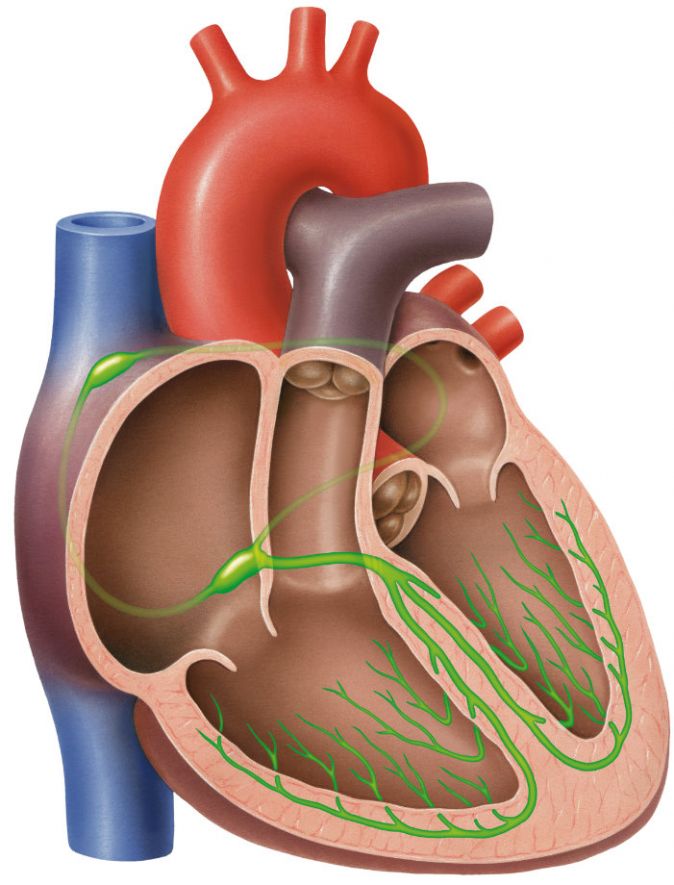
Cross-section of the heart: In green at the top of the right ventricle is the sinus node, which sends impulses to the heart chambers via the conduction system © lom123 | AdobeStock
In atrial fibrillation, there is an excessive number of circling electrical impulses in both atria, which are formed outside the sinus node. These uncoordinated signals are unable to cause normal muscle contraction. As a result, only a small proportion of the signals reach the ventricles, as the conduction of excitation is additionally blocked.
A slow arrhythmia occurs. Atria and ventricles cannot fill with enough blood. If the patient also suffers from heart failure, the heart muscle pumps even less blood through the body. As a result, the blood pressure drops.
If the sinus node generates a high number of electrical impulses, they cause heart palpitations (too fast arrhythmia) in the ventricles below.
In the early stages, atrial fibrillation only occurs in fits and starts. After a few minutes or at most hours, the heart rhythm returns to normal on its own.
With regard to the exact causes of the cardiac arrhythmia, there is still a considerable need for research. Doctors assume that the altered heartbeat is caused by age-related scarring of the heart tissue. It is no longer able to transmit the electrical impulses as required. The signals circulating in the atrium negatively influence normal heart activity.
In addition, the risk of developing atrial fibrillation at an older age seems to be genetically determined. However, sometimes it develops spontaneously without any other cause.
Factors that favour the disturbed heart rhythm are for example
People who experience one or more of the above signs should contact a specialist as soon as possible. Suitable contact persons are specialists for internal medicine or cardiologists. The same applies if the atrial fibrillation does not disappear on its own within two days at the latest.
The irregular heartbeat can be diagnosed with the help of a blood pressure measurement and an ECG (electrocardiogram). The doctor sticks electrodes on the affected person's chest that measure their heartbeat. If atrial fibrillation is suspected, a stress ECG or a long-term ECG is used.
The stress ECG is used to measure the heart flows under physical stress, i.e. increased pumping activity of the heart. The patient sits on an exercise bike and pedals hard.
The long-term ECG is about measuring the heart's electrical activity over 24-48 hours. For this purpose, the patient carries a small mobile ECG device. It records the heart activity in the patient's daily life.
The physician evaluates the data after the measurements are completed.
Paroxysmal atrial fibrillation is easy to record with an event recorder. The patient only activates the device when the atrial fibrillation becomes noticeable. The doctor then analyses the data on the PC.
The echocardiogram (ultrasound image of the heart) provides detailed information about the condition of the heart muscle and its pumping behaviour. In addition, the examining specialist can easily recognise any blood clots that may be present.
An ultrasound probe connected to a narrow tube is used to perform an echocardiogram. The doctor pushes this through the mouth and throat to the middle of the oesophagus of the patient. From there, the doctor can take a close look at the right atrium of the heart. The patient is given a mild sedative beforehand.
If the cardiac arrhythmia is due to a thyroid disease, the specialist will treat only this first. After that, the atrial fibrillation usually improves all by itself.
In paroxysmal atrial fibrillation, the doctor prescribes special medication called antiarrhythmics. The patient takes it as soon as he feels an attack coming on. Antiarrhythmics bring the heart rate down to a resting pulse of about 70 beats per minute within a short time.
However, the patient must be careful to take the medication exactly as instructed: Accidental overdoses can greatly slow down the heartbeat. Atrial fibrillation accompanied by palpitations can also be treated effectively with medication.
To minimise the increased risk of stroke, the patient is also given blood-thinning medication, such as Marcumar or Xarelto. They prevent the blood circulating in the atrium from clumping together and forming blood clots. These could then be sent to the brain where they could clog an important blood vessel.
Drug therapy does not always work. If the heart patient continues to have symptoms, electrocardioversion (electric shock treatment) is recommended. For this purpose, the patient is connected to various devices under short-acting anaesthesia. They control the blood pressure and the oxygen supply. Two applied electrodes then conduct current through the heart muscle for fractions of a second. This causes the heartbeat to normalise.
Most often, it is the connection points between the pulmonary veins and the heart that trigger the disease in the patient. In this case, the patient can also be treated with pulmonary vein isolation (catheter ablation).
To do this, the doctor inserts a catheter (thin plastic tube) through a small incision from the groin vein through the great vena cava to the left atrium. There he scleroses the muscle tissue that causes the arrhythmia with the help of high-frequency current or cold.
6 to 8 out of 10 patients become permanently symptom-free through catheter ablation. Repeating the procedure further increases the chances of recovery for those affected.
The German Heart Foundation advises that this operation should only be carried out in a special heart centre. This reduces the risk of complications occurring due to the great experience of the doctors involved. In addition, an inserted pacemaker significantly improve the patient's heart function.
Patients with heart disease who also have atrial fibrillation sometimes suffer relapses after successful treatment. People with heart failure who develop atrial fibrillation in the course of their lives usually die earlier than patients who only have cardiac arrhythmias.
The occurrence of atrial fibrillation cannot be prevented in principle. However, it is quite possible to prevent the development of the underlying diseases of which the cardiac arrhythmia is a direct consequence.
Since narrowed coronary arteries are the main cause of the disease, it is recommended,
- to eat healthily,
- to do enough sport and
- as far as possible, no smoking and
- excessive drinking
zu verzichten.