Recommended specialists
Brief overview:
- What is a cruciate ligament tear? A partial or complete tear of the anterior or posterior cruciate ligament in the knee. Knee stability is impaired as a result. The anterior cruciate ligament is affected more often than the posterior.
- Causes: An accident while playing sports is almost always the cause, but work and traffic accidents can also cause a cruciate ligament tear.
- Symptoms: Severe pain, a tearing or shifting sensation with a cracking sound at the moment of the accident. Afterward, a hematoma, bruising and swelling of the knee joint, and knee instability may occur.
- Diagnosis: In addition to performing a movement test, the patient’s medical history and a knee examination allow for a diagnosis. In addition, X-ray and MRI examinations are often also used for diagnosis.
- Treatment: Conservative methods include muscle building, physiotherapy, pain and cold therapy. These methods may alleviate the symptoms but they don’t repair the cruciate ligament.
- Surgery: In the course of a surgery performed mainly arthroscopically, the defective cruciate ligament is replaced by an intact tendon from the patient's own body.
- Surgical aftercare: During rehabilitation, the patient should learn to straighten and bend their knee again as quickly as possible. They are usually on sick leave for 14 days. This is followed by rehabilitation and running training.
- Prognosis: After surgery, the long-term prognosis is generally good, but osteoarthritis can still develop later on.
- Prevention: the risk of injury can be minimized by means of strength, proprioception, and coordination training as well as protective reflex exercises. A knee brace can also help.
Article overview
- Definition: What is a cruciate ligament tear?
- What are the causes of a cruciate ligament tear?
- What are the symptoms of a cruciate ligament tear?
- Diagnosing a cruciate ligament rupture
- Treating cruciate ligament ruptures
- Surgically treating cruciate ligament ruptures
- What is the aftercare following surgery?
- Prognosis for cruciate ligament ruptures
- How can you prevent a cruciate ligament tear?
Definition: What is a cruciate ligament tear?
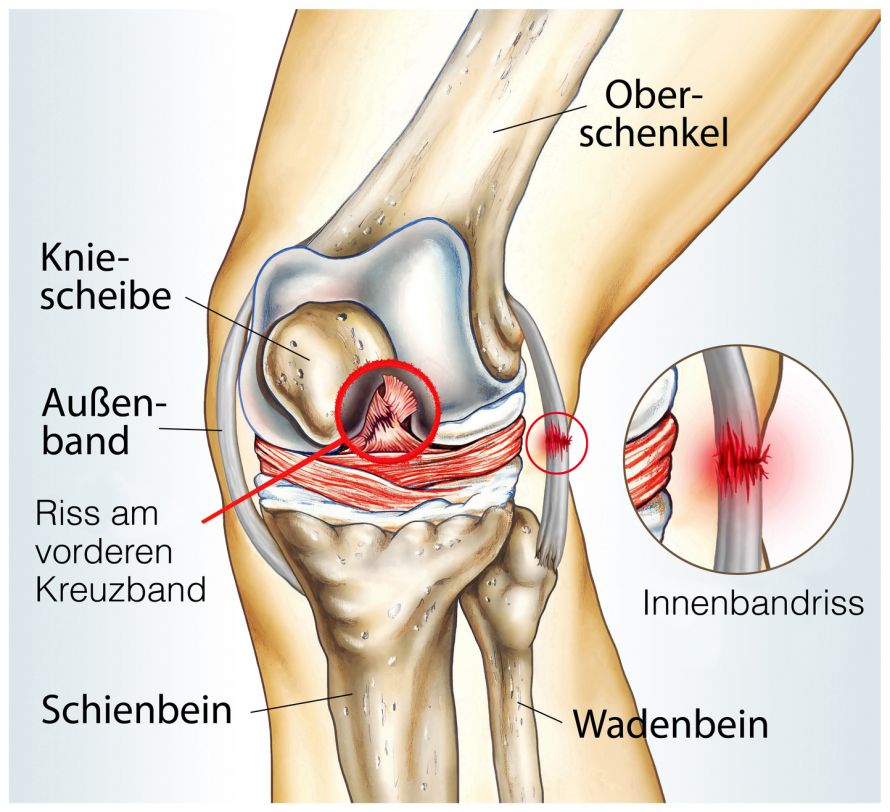
A cruciate ligament tear (ICD code: S83) is a partial or complete tear of a cruciate ligament in the knee joint. Both the anterior and posterior cruciate ligaments may be affected. Accordingly, a distinction is made between an anterior and a posterior cruciate ligament tear.
According to the Federal Statistical Office of Germany, an anterior cruciate ligament tear is diagnosed 35,000 times a year in Germany. This injury is therefore one of the most common and at the same time one of the most serious knee joint injuries.
The cruciate ligament is one of the two central stabilizers of the joint. The anterior and posterior cruciate ligaments are positioned centrally in the knee joint. They stabilize the joint and almost the entire range of motion when running, walking, and jumping.
The failure of the cruciate ligament results in increased lower leg advancement. The remaining internal knee components must then assume the function of stabilization. The result is often further damage to the meniscus, ligaments, and articular cartilage.
In the following video you can see the anatomy of the knee joint:
What are the causes of a cruciate ligament tear?
People between the ages of 15 and 30 are most commonly affected as this age group is very active in sports. Women have an injury rate up to eight times higher than that of men.
- Hormonal influences,
- Anatomical differences, and
- Differentiated training procedures
have been discussed as possible causes for this difference. Every third cruciate ligament rupture occurs at the same time as a meniscus injury. Concomitant ligament and articular cartilage injuries are also common.
In most cases, a cruciate ligament rupture results from a sports accident, especially in sports like
- Soccer,
- Handball, and
- Skiing.
However, work and traffic accidents are also common causes of cruciate ligament rupture. Anterior cruciate ligament (ACL) injuries often occur without direct external impact (>70% of injuries).
Typically, a cruciate ligament tear occurs due to unforeseen changes in direction. High acceleration forces, e.g., during skiing, lead to an external rotation of the lower leg at the bent knee joint and at the same time to an opening of the joint at its inner side (so-called valgus stress). The otherwise stable ligament can no longer withstand the forces acting on it.
- Inward rotations with tilting to the outside (so-called varus stress) and
- Strong stretching and bending movements
can also lead to a cruciate ligament rupture.
© Henrie / Fotolia
The typical mechanism of injury is the sudden and unexpected change of direction with twisting of the body while stopping the walking speed. The foot is fixed to the floor. Contact with an opponent is not required. We refer to this as injury from twisting while standing firm.
What are the symptoms of a cruciate ligament tear?
The cruciate ligament tear manifests itself
- In severe pain and
- By a tearing or shifting sensation in the knee that is heard as a crack.
A bruise quickly forms: A sensation of tightness and stress pain develops.
Without immediate ice and compression treatment, the knee swells quickly due to
- Hemarthrosis from the arterial supply of the anterior cruciate ligament rupture, and
- Hemorrhaging into the peripheral soft tissues due to capsular injuries.
A swollen knee (joint effusion) can also occur.
In most cases, those affected are then unable to continue playing sports.
These acute symptoms of an anterior cruciate ligament tear usually subside within 10 to 14 days. The joint can then be subjected to loads like normal again. Throughout the injury, the affected person often experiences a feeling of instability and insecurity in the knee joint. The load-bearing capacity of the joint also increasingly decreases in everyday life. The following are characteristic symptoms:
- Uncertainty when walking,
- A spontaneous buckling of the knee joint,
- Load-dependent pain, and
- An inhibition against extending and flexing the knee joint.
At some point, the persistent instability leads to secondary damage to the meniscus and articular cartilage. Up to 80 percent of those affected suffer a meniscus tear five to ten years after their cruciate ligament rupture, injuring another joint stabilizer. This increasing instability often leads to an arthrosis later on.
Diagnosing a cruciate ligament rupture
To diagnose an anterior cruciate ligament (ACL) tear, the first step is to review the medical history (anamnesis), that is, to talk to the doctor.
Medical history interview
As part of the anamnesis, the attending physician asks the affected patient the following questions:
- Is the current knee trauma actually a first-time accident or was it already preceded by a first-time accident?
- Was the knee already swollen after previous twisting traumas, has it already made a cracking noise before, did the patient have to stop a sporting activity because of an acute injury to the same knee joint?
- Was there a puncture with bleeding?
- Did the injured person receive a cast or a bandage?
- After the incident, was the knee not as stable as the healthy knee?
- Throughout the injury progression, did swelling repeatedly occur with minor twisting?
The five most important questions about the symptoms are:
- Is there severe pain from deep inside the joint?
- Was there a cracking noise (a very reliable sign if affirmative, but can occasionally go unnoticed)?
- Was there swelling, effusion (1-24 hours after trauma)?
- Did you stop participating in the game or sport (skiers can still occasionally finish runs due to the effects of the cold)?
Positive responses to some of these questions suggest a previous ACL injury. A feeling of instability with a tendency to subluxation is evidence of chronic anterior cruciate ligament insufficiency.

© westfotos.de / Fotolia
Clinical examination of the knee joint
The physician will thoroughly inspect and feel (palpate) the patient's injured knee. Fresh skin lesions indicate the type and intensity of the injury. At the point that the examiner detects scars from an injury and surgery, they should look for the patient’s medical history.
A malalignment of the leg axes is very important for the prognosis. Varus malalignments in combination with posterolateral capsular ligament injuries, for example, lead to instabilities with considerable handicap for the patient.
The active and passive movement tests complete the physical exam. The doctor uses palpation and certain movement patterns to check
- The areas of pain around the knee joint and
- The functioning of the ligaments.
Imaging techniques
In addition, imaging procedures are usually used, such as X-rays and magnetic resonance imaging (MRI). However, these procedures are restricted for patients with previous knee joint operations with metal parts.
Standard X-rays, preferably those comparing the uninjured with the injured side, can confirm an old cruciate ligament injury based on
- Osteophytes,
- Incipient condylar flattening,
- Joint cavity narrowing, and/or
- Clumping of the cruciate ligament tubercles.
Another diagnostic test from the field of radiology is the scintigraphy. It has gained importance in recent years for its detection of "active" cartilage/bone lesions in the knee joint. Thus, "hot spots" indicate active areas of chondromalacia with cell death.
Chondromalacia means cartilage damage of the joints. If possible, unstable knee joints with hot spots should be stabilized to slow the progression of these cartilage disorders.

X-rays can be used to determine whether the bony structures have suffered damage after a cruciate ligament tear © angkhan | AdobeStock
Treating cruciate ligament ruptures
A cruciate ligament tear can generally be treated both conservatively and surgically.
Conservative therapy methods include, but are not limited to
- Physiotherapy to stabilize the knee joint and build up muscles,
- Pain management, and
- Cold therapy.
The mostly younger patients very often desire to continue being active in sports. In principle, this is conceivable even without a functional anterior cruciate ligament if the knee joint has good muscle control.
But one should not be deceived: Due to possible secondary damage, only about one in two affected persons can actually participate in their sport without any restrictions five years after a cruciate ligament rupture. In addition, the long-term muscle development that is often intensively carried out for decades is rather unlikely.
The anterior cruciate ligament should therefore be surgically stabilized after a cruciate ligament tear as part of a cruciate ligament surgery. Incidentally, this also applies to children and the elderly and not only young adults.
Surgically treating cruciate ligament ruptures
The modern arthroscopic techniques have completely replaced the older surgical technique, which required opening the entire joint. Techniques in which the torn cruciate ligament was sewn back together are also obsolete today.
Instead, the injured cruciate ligament is replaced with a tendon from the patient's own body. You can see a cruciate ligament reconstruction procedure in the video:
When should surgery for a cruciate ligament tear be performed?
The ideal time for performing reconstruction surgery after an anterior cruciate ligament tear is disputed. To avoid complications during surgery, many surgeons wait at least four to six weeks for isolated cruciate ligament injuries.
If the body's own healing process has not yet begun in the injured joint, the procedure can also be performed immediately after the cruciate ligament tear.
Concomitant injuries also often determine the right time. Meniscus injuries in particular are frequent and should then be sutured promptly, if this is at all technically possible.
What material is used during the operation?
The patellar tendon and the semitendinosus tendon are the primary materials used for replacement surgery in the case of a cruciate ligament rupture. The use of the patellar tendon is the gold standard. Various surgeons also primarily use the quadriceps tendon.
All grafts may present problems in their surgical application. What's really important is the correct placement of the replacement tendon in the knee joint. This must be positioned as precisely as possible in the same place as the original cruciate ligament. This is the only way to ensure that the knee joint can be subjected to loads and moved almost to its full capacity after a cruciate ligament rupture. The correct placement is technically demanding for the orthopedist.
How is surgery performed for a cruciate ligament tear?
In most cases, a single tendon cord is inserted into the knee joint as a graft. This is referred to as a single-bundle technique.
However, this does not correspond to the anatomical specifications: The cruciate ligament actually consists of three individual main fiber bundles. These are helically twisted into each other. Biomechanical studies suggest that the anteromedial and posteromedial bundles provide the main guidance.
Therefore, a more advanced surgical technique has evolved over the past few years that no longer uses a single bundle. Instead, two slightly narrower grafts are used, but they are inserted more in the original course of the two fiber bundles.
This modern double-bundle technique is primarily intended to prevent the unpleasant postoperative rotational instability that can occasionally remain after conventional techniques.
However, this advantage, which has not yet been completely verified, is offset by
- Greater surgical complexity,
- Procedural complications,
- Higher costs, and
- Increased complexity in case of revision surgery.
This technique is currently still the subject of scientific discussion and does not yet represent a routine procedure. Nevertheless, this therapeutic approach is extremely promising and represents a serious alternative in modern cruciate ligament surgery.
What is the aftercare following surgery?
The severity of the knee injury is also evident in the aftercare following a cruciate ligament tear. In this context, rehabilitation is considered the most important measure to ensure the success of the operation in the long term.
Cruciate ligament tear surgery must be followed by early functional aftercare. The goal is to extend the knee joint as quickly and completely as possible and to achieve a bending capacity of up to 120°.
After 14 days, the patient is cleared to go back to work, at least for office work. Proper and time-consuming rehabilitation takes much longer. It may well be completed after eight to ten weeks or take even longer.
This is almost always followed by further individual rehabilitation training. Thus, light running training is usually only possible after three months. The resumption of sports that put a strain on the knee is recommended after six months at the earliest.

Rehabilitation is important for good results after cruciate ligament tear treatment © AYAimages | AdobeStock
Prognosis for cruciate ligament ruptures
Overall, the long-term prognosis of properly performed cruciate ligament replacement surgery is good: The stability of the joint is ensured for years.
However, the development of osteoarthritis in the injured joint cannot always be prevented. Despite a successful operation, the prognosis depends decisively on the previous existing damage and the accompanying meniscus injuries.
However, only a stabilized joint has a chance of being truly protected from this.
How can you prevent a cruciate ligament tear?
The risk of suffering a cruciate ligament rupture can be countered by means of
- Strength training,
- Proprioception training, and
- Coordination training.
This makes it possible to optimize everyday or sport-specific movement sequences in unfamiliar stress situations.
Training protective reflexes through balance exercises is very helpful for stabilization in extreme situations. These include unforeseen events such as stumbling or events demanding a high degree of muscular coordination, such as a fall while skiing.
The trained muscles surrounding the knee joint are capable of absorbing large loads if they are activated in a timely and properly coordinated manner. In the case of an excessive load or the unexpected application of force, the load is transferred directly to the ligaments of the knee. Gaining time to give the muscle a chance to intervene is the most important protective factor in this phase to counteract trauma-related strain and damage such as a cruciate ligament tear.
In addition to preventive training, using a prophylactic knee brace to prevent a cruciate ligament tear is also subject to discussion. An orthosis (brace) must be aligned with the sport practiced in terms of appropriate design and use. Movement patterns and injury mechanisms can vary greatly between different sports.
Thus, sports such as soccer or American football are not comparable with ice hockey. Soccer and American football require increased fixation of the leg to the ground (cleated shoes). In ice hockey, on the other hand, the aim is to achieve reduced friction with reduced fixation to the surface (ice).
Meanwhile, more than 100 prophylactic splints have been fitted in ice hockey players during our 10-year prospective study. They produced consistently positive results. According to our experience with the national ice hockey team, the use of orthoses should be advocated as a prophylaxis against a cruciate ligament rupture and other injuries in this sport.