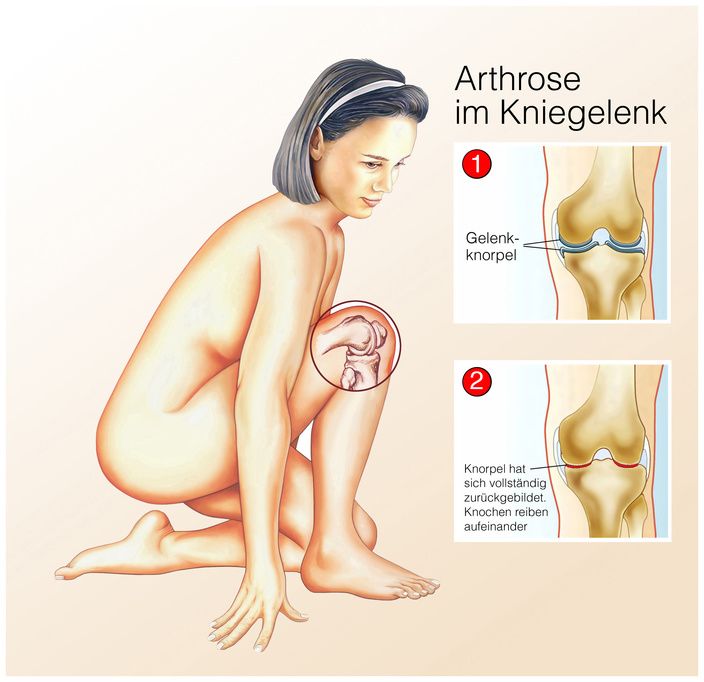
Knee osteoarthritis is the breakdown of cartilage in the knee joint. The wear and tear causes knee pain and limited mobility.
It is diagnosed based on a physical exam and evidence of joint changes on an X-ray. In addition to conservative procedures, surgical treatment is also available.
An overview of the knee joint and its structure with cartilage and ligaments is shown in the video:
All joints of the body can be affected by osteoarthritis, i.e., the degradation or wear of the cartilaginous joint surfaces.
The knee is subjected to particularly high stresses. That is why it is often affected by osteoarthritis. Knee osteoarthritis is also called gonarthrosis.
Due to the friction of the joint, the cartilage becomes increasingly rough and gradually degrades. In severe cases, parts may detach from the bone or cartilage. The video shows how knee osteoarthritis including cartilage damage develops:
As a result of this degradation process, the joint cavity narrows, resulting in both knee pain and inflammation and swelling in the knee joint. This reduces the mobility of the joint.
Depending on the affected area of the joint, a distinction is made between these types of gonarthrosis:
- Patellofemoral osteoarthritis: Wear and tear in the joint of the kneecap (patellofemoral joint).
- Medial tibiofemoral osteoarthritis: Damage to the internal (medial) tibiofemoral joint (the joint between the femur and tibia). This is referred to as varus gonarthrosis if there is additional varus malalignment.
- Lateral tibiofemoral osteoarthritis: Damage to the external or lateral aspect of the tibiofemoral joint. If there is simultaneous valgus malalignment, it is referred to as valgus gonarthrosis.
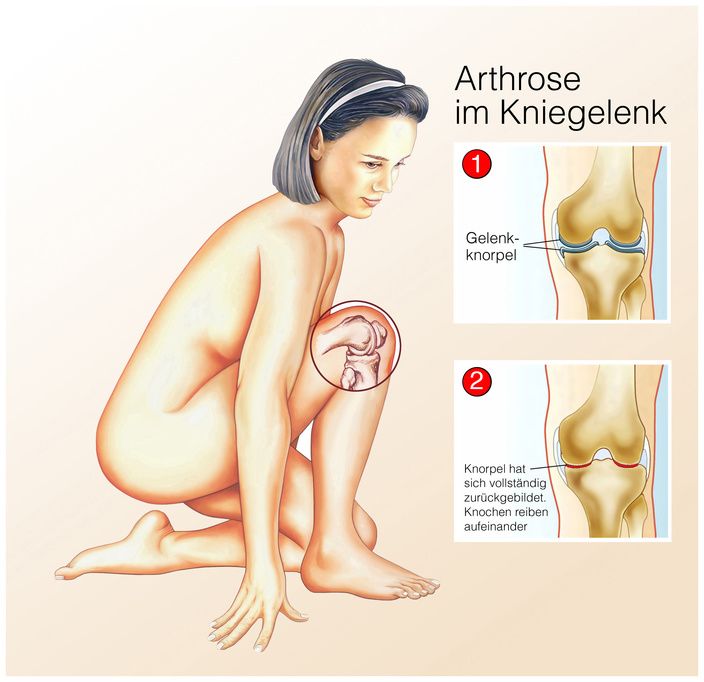
In knee osteoarthritis, the joint cartilage is worn © Henrie / Fotolia
In all people, signs of wear and tear in the knee joint (primary osteoarthritis) occur with increasing age. However, not only age is considered a risk factor for the development of knee osteoarthritis, but also
- Hereditary factors
- Being overweight,
- Excessive or one-sided physical or athletic strain,
- Deformities,
- Injuries, and
- Inflammation.
One speaks of secondary knee osteoarthritis when the gonarthrosis is the result of
- An injury,
- Illness, or
- excessive load.
The typical symptom of gonarthrosis is knee pain that occurs with exertion. In the advanced stage, the mobility of the knee joint becomes increasingly limited. Swelling occurs in the knee, the patient limps and assumes a relieving posture.
Depending on the symptoms, knee osteoarthritis can be divided into three stages:
- Stage 1: No symptoms. Osteoarthritis is usually detected only by the changes on the X-ray.
- Stage 2: Start-up pain that increases with exercise and improves at rest.
- Stage 3: Persistent pain, even at rest. There are also significant restrictions on movement.
The condition is diagnosed based on
- A detailed anamnesis (patient consultation regarding the symptoms and triggers),
- A physical exam (assessment of gait, range of motion, leg axis, and leg length),
- Functional tests (e.g., ligament stability),
- Pain tests, and
- X-rays of the knee joint.
In some cases, special examinations such as
are performed. An arthroscopy of the knee joint is an important tool for the diagnosis and the simultaneous treatment of the damage. The video shows a knee arthroscopy procedure:
Depending on the stage, therapy is either conservative or surgical.
Conservative treatment of knee osteoarthritis consists of several treatment steps:
- Lifestyle adjustment (for example, reducing body weight, if necessary, and to avoid incorrect loading),
- Physical measures (e.g., hot or cold treatment),
- Physiotherapy,
- Orthopedic aids,
- Medication for pain relief,
- Acupuncture, if necessary.
In terms of surgery, knee surgery can be divided into joint-preserving, joint-stiffening, or joint-replacing knee surgery.
In some circumstances, an arthroscopy may be sufficient for cartilage smoothing and partial removal of concomitant meniscal damage. Clearly-defined cartilage lesions must be present for this to occur. This procedure can provide years of pain relief for the patient.
Axis corrections can lead to a more favorable distribution of pressure in the knee joint at earlier stages of osteoarthritis.
In the case of advanced knee osteoarthritis, the only remedy is often prosthetic treatment. The patient then receives an artificial knee joint (knee prosthesis).
Specialists for knee osteoarthritis are usually specialists for orthopedics, sports medicine, or rheumatology.
Other exams (MRI, CT scans) are performed by specialists in the fields of radiology/nuclear medicine.
Clinics for knee osteoarthritis are clinics for
- Orthopedics,
- Sports Medicine,
- Endoprosthetics, and
- Knee Surgery.