Recommended specialists
Brief overview:
- Anatomy: Meniscuses are buffer discs in the knee joint, which are responsible for transmitting pressure, absorbing shock, and stabilizing the knee.
- What is a meniscus tear? If the meniscus tears, it can no longer fully perform its function; this may result in discomfort and premature knee osteoarthritis.
- Causes: A meniscus tear can be accidental or degenerative. Sports injuries, accidents, overexertion, but also wear and tear can cause a meniscus tear.
- Symptoms: Pain when twisting, squatting deeply, and at night, as well as knee instability and other sequelae.
- Diagnosis: A torn meniscus is simple to diagnose. If there is any uncertainty, an X-ray and an MRI will provide clarity.
- Surgery: Surgery takes place arthroscopically, i.e., it is minimally invasive. The exact procedure depends on which meniscus is affected and where exactly the tear is located. In principle, resection, partial resection, a meniscal suture, and a meniscal implant are conceivable. Detailed information is provided in the text below.
Article overview
Anatomy and function of the meniscuses
The knee joint is the largest joint in our body and it is also the joint subject to the most strain. It connects the upper leg with the lower leg. As a result, it transfers the entire load of the trunk to the lower leg.
The meniscuses are two crescent-shaped discs of fibrocartilage. They are located in the knee joint between the upper and lower leg bones. There is a lateral and a medial meniscus.
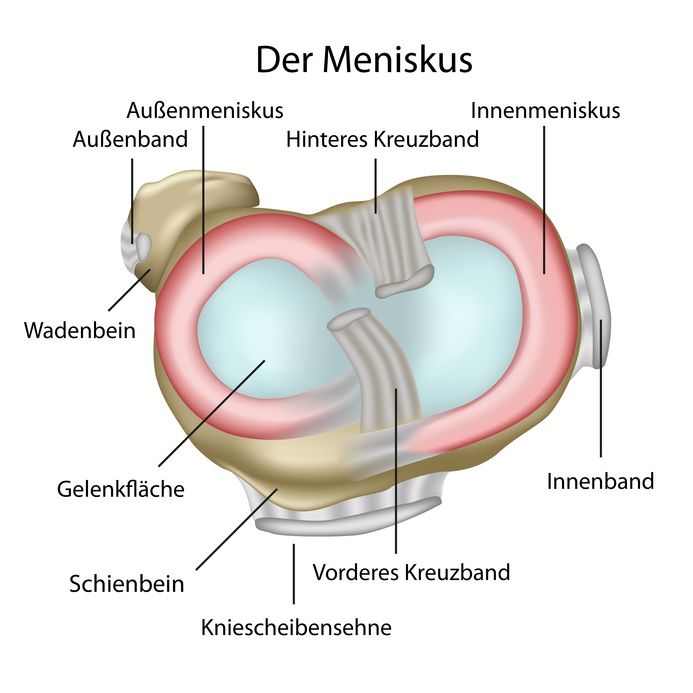
Cross section of the knee joint: Meniscuses seen from above © bilderzwerg / Fotolia
The meniscuses play an extremely important role in the function of the knee joint. It is particularly crucial that they
- Transfer the load from the upper to the lower leg and
- Stabilize the knee during flexion, extension, and rotation.
Together with the cruciate ligaments, the meniscuses ensure synchronous rolling and sliding of the femoral condyles on the tibial plateau.
Other functions of the meniscuses include:
- Distributing the load on the joint surfaces,
- Absorbing shock,
- Contributing to the lubrication and nutrition of the joint.
Because of these important functions, it makes sense from a medical point of view to maintain the meniscus for as long as possible.
Watch the video below to see the structure of the knee joint and where the meniscuses are located:
How does a meniscus tear occur?
The meniscuses are not completely permeated by blood vessels. They are only well supplied with blood in their peripheral zone, the so-called red zone. These small blood vessels do not reach the center of the meniscus.
Therefore, this non-vascularized white zone of the meniscus is supplied with nutrients only by the synovial fluid. If the meniscus has too few nutrients and fluid, it becomes dry and brittle and degenerates. Damage becomes more likely and the cracks cannot heal on their own.
Basically we distinguish between
- Traumatic (accidental) and
- Degenerative (due to wear and tear or overload)
causes of meniscus tears.
Fresh, traumatic meniscus tears tend to occur in sports injuries. Very great forces often act on the knee joint, especially during sports activities involving twisting and shearing movements. These forces lead to excessive strain and painful injuries in the knee joint, especially in the
- Cruciate ligaments,
- Cartilage surfaces, and
- Meniscuses.
Combined injuries of the cruciate ligament and meniscus (cruciate ligament tears, MCL tears, and meniscus tears) are also common.
© bilderzwerg / Fotolia
Degenerative meniscus damage accounts for the majority of meniscus tears. The meniscuses are often chronically overloaded over many years, for example, due to unfavorable loads
- When performing deep squats,
- Being overweight,
- When performing repeated twists.
Many minor instances of excessive strain during sports or work also wear down the meniscus tissue. Eventually, this can cause the pre-damaged tissue to tear in the event of a single overload.
- Pain,
- Blockages, and
- Swelling
are the result.
If left untreated, the torn parts of the meniscus will keep getting caught between the joint surfaces of the thigh and lower leg. The cartilage of the joint surfaces is permanently damaged by these impingements. If this mechanism is not stopped by surgery, osteoarthritis (joint wear) of the affected joint section will develop over time.
Symptoms and diagnosis of a torn meniscus
In sports injuries that damage the meniscus, the accident already gives a direct indication of the meniscus damage. Typical signs of meniscus tears are:
- Pain when twisting,
- Pain when performing deep squats, and
- pain at night, especially when the knee joints are on top of each other.
Experienced physicians can make a suspected diagnosis of a meniscus tear with relative certainty by a medical exam. X-rays can be used to rule out damage to the bone.
If the findings are unclear, magnetic resonance imaging (MRI) can reliably detect meniscus damage.
Meniscus tear surgery
A torn meniscus leads to knee instability and subsequently to excessive joint wear (osteoarthritis). Therefore, surgical stabilization as early as possible is essential.
As a rule, fresh meniscal tears close to the base can be properly treated by a surgeon using arthroscopic sutures or suture systems. The affected area grows back and again develops intact meniscus tissue from fibrocartilage.
Torn meniscuses are operated on arthroscopically. The video shows the procedure of this minimally invasive surgery:
Arthroscopic treatment of meniscal damage is now an established and routine procedure. It is performed in many orthopedic clinics and surgery centers.
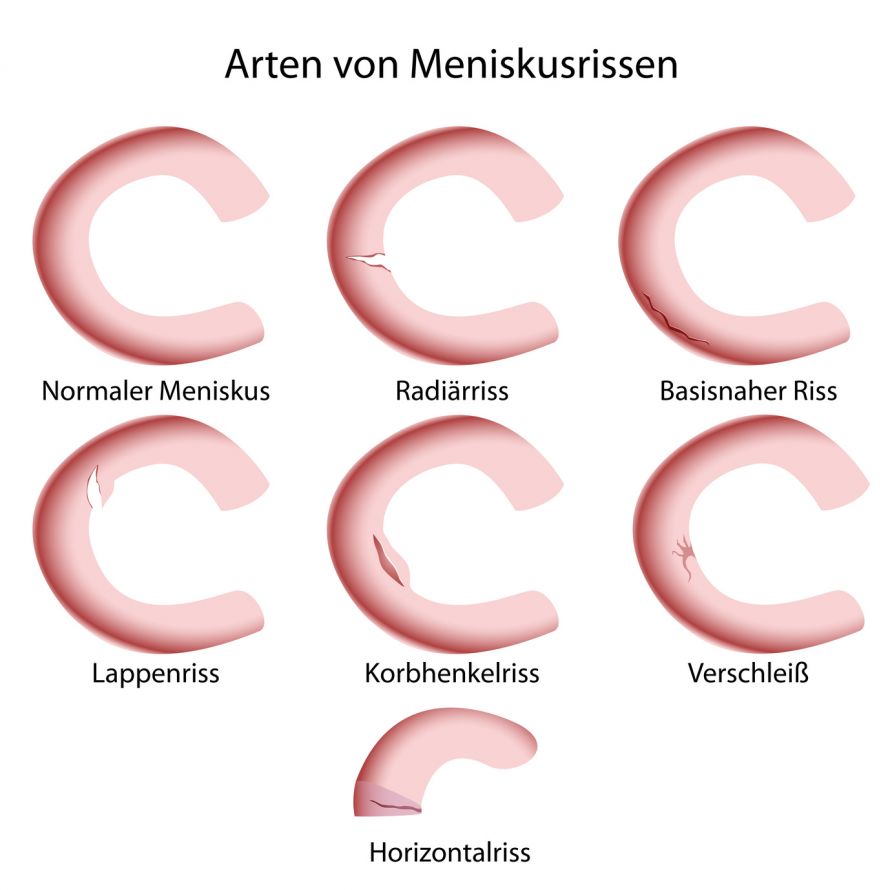
The options for surgical treatment depend on the type of torn meniscus. The localization and freshness of the tear are also important.
Meniscus resection and partial resection
The motto for meniscus surgery is: Remove as little tissue as possible, but as much as necessary. All potentially damaging parts of the meniscus are removed using special instruments. In most cases, no more than 1/3 or 2/5 of the meniscal substance needs to be removed.
Most meniscus tears are degenerative in nature (wear and tear damage). Repair (suturing) is then no longer possible and the torn tissue must be removed.
By means of arthroscopy, it is possible to very gently remove the damaged meniscus tissue (resection). It is a short procedure that is usually performed under light general anesthesia or epidural anesthesia.
A miniature camera is inserted into the knee joint through a small skin incision. It can be used to examine the affected knee. Surgical instruments and any necessary implants are gently inserted into the joint via other tiny access points. In this way, the surgeon can repair the injured structures.
Nowadays, such operations are generally very low impact on the patient.
Health and the conditions at home permitting, the surgery can be performed on an outpatient basis. The patient can then leave the recovery room about two hours after the operation, accompanied and with the help of forearm crutches.

Knee arthroscopy does not require long skin incisions © smartmediadesign | AdobeStock
Partial meniscus resection aftercare
After surgery, a soft padding bandage and an elastic compression bandage are applied. The dressing is comfortable and can absorb fluid from the arthroscopy and residual blood from the puncture sites. A small tube may be inserted into the joint to drain wound fluid.
The bandage is removed the day after surgery and replaced with waterproof band-aids that protect the wound until the stitches are removed a week later.
Your knee joint should be cooled with ice and elevated to minimize swelling. During the first few days after surgery, the small puncture sites, approximately 5 mm wide, may be somewhat sensitive. The sensation of "trickling" fluid in your knee joint is not a cause for alarm. It is residual fluid from the arthroscopy and will disappear on its own.
You may shower carefully with the waterproof band aids. Bathing and swimming should be avoided for 10 days to prevent water from getting into the joint from the outside. You will need crutches for some time after surgery. As a rule, however, it is possible to occasionally put approximately 30 kg of weight on the operated leg on the first day after surgery.

Walking aids are necessary in the period after surgery © S Amelie Walter | AdobeStock
Isometric tensing exercises should be started immediately. They are performed every hour and help maintain the thigh muscles. You should avoid saunas/sunbeds for three weeks after surgery (risk of swelling).
Running is possible from the fourth week after surgery and stop-and-go sports from the sixth week. In general, the rule, of listening to your knee applies. Increase all loads slowly and feel how the joint reacts.
Be careful not to subject the knee to impact loads (hard heels) for the first few weeks after surgery. Especially in older people, fatigue fractures can occur after too much stress following a meniscus surgery.
Meniscus surgery: Suturing the meniscus
In the case of fresh meniscus tears in the rim supplied by blood, it is possible to re-suture the torn meniscus. This applies in particular to bucket handle tears.
Certain areas of the meniscus are difficult to reach and the nerves and blood vessels in the back of the knee must not be damaged. Therefore, special suturing instruments are required for refixation in the posterior horn area of the meniscuses.
Meniscus refixation is also now performed arthroscopically in a minimally invasive manner.
The aftercare following meniscal suturing is considerably more complex than meniscal resection:
Some weight (10-20kg) may be put on the knee for three weeks with two forearm crutches and while wearing a stabilizing splint with temporary limitation of movement.
The knee may not be loaded when bending the knee deeply and no knee-straining sports are allowed for three months.
On the other hand, the following are permitted
- Cycling,
- Crawl swimming from the fourth week, and
- Jogging from the eighth week.

Swimming is one of the sports that may be resumed quite quickly after meniscus surgery © Microgen | AdobeStock
Meniscus surgery: Meniscus implants
Many injuries can no longer be sutured. In these cases, the tear is located in the part of the meniscus that is not supplied by blood or the tissue is already irreparably destroyed.
Studies have shown that even partial removal of meniscal tissue can lead to increased stress. This can lead to degenerative changes in the articular cartilage. As a result, there is a high probability of developing knee osteoarthritis later. This is associated with significant pain and restrictions in movement.
An international team led by the well-known American sports physician Dr. Steadman has developed a biological implant for such cases. It stimulates the body to form meniscus-like tissue, thereby filling the defect.
How does the meniscus implant work?
The meniscus implant is biological and resorbable. It consists of highly purified collagen with a sponge-like structure or a polyurethane scaffold (suppliers ReGen Biologics: Menaflex and Ormed-DJO: Actifit). The shape is based on the human medial or lateral meniscus.
The implant is arthroscopically sutured in place of the removed meniscal tissue. It then uses the body's ability to regenerate its own tissue. The porous structure of the implant serves as a guide for the ingrowth of new tissue.
The body's own cells gradually migrate into the implant and form meniscus-like tissue. After approximately one year, most of the collagen meniscus implant (CMI) is degraded and replaced by the patient's own tissue.
Clinical experience with the meniscus implant
The results from clinical trials in the USA and Europe show that the meniscus implant supports the growth of new tissue. The pain that was previously present is significantly reduced and patients return to a similar level of activity as before the injury.

© westfotos.de / Fotolia
The CMI was first introduced for operations on patients as part of a feasibility study in the USA in 1993. The positive results led to the initiation of multicenter studies in the U.S. and Europe in 1997. Based on the positive results, the CE mark of conformity was issued in 2000 for the medial implant. In the meantime, the CMI for the lateral meniscus has also been approved in Europe and is in clinical use.
The American multicenter study with more than 300 patients also proves the advantageousness of the CMI regarding
New formation of meniscus tissue,
- Pain reduction,
- Reaching the usual level of activity, and
- Satisfaction of treated CMI patients compared to patients who had only part of their meniscus surgically removed.
The average operation time of CMI implantation is comparable to that of a complex meniscus refixation.
Chances of success with the meniscus implant
To date, more than 1,400 patients worldwide have undergone successful CMI implantation surgeries. These were mainly people who placed great emphasis on regaining their athletic activity. In about 90 percent of treated CMI patients, the intended treatment success can be demonstrated by clear tissue regeneration.
After treatment, these patients have an average of 70 percent of their original meniscus substance back. This was the result of a randomized multicenter study (USA) with more than 300 patients.
The implant becomes more and more resistant as the body's own cells grow in. To guarantee success, the patient must consistently adhere to the specific rehabilitation program at all times.

With a meniscus implant, patients can return to sports activities similar to those before the injury © Dudarev Mikhail | AdobeStock
Who can benefit from meniscus implant treatment?
The following requirements should also be met from a medical point of view:
- The present meniscus tear cannot be treated otherwise.
- For correct suturing, a predominantly intact meniscal rim and stable meniscal ends must be present.
- The size of the injury is at least 35 percent of the meniscus substance.
- There is little or no articular cartilage damage.
- There should be no malposition of the leg axis, otherwise it must be corrected before or at the latest at the same time as the meniscus implantation.
- No capsule or ligament instabilities are present.
- The patient is motivated and has a sufficient amount of time for the recommended aftercare.
Meniscus implant aftercare
Aftercare extends over a total period of approximately six months. Initially, the load and the extent of movement must be increased slowly and continuously. After two months, the operated knee can usually be fully loaded again. The patient must now start retraining for their usual sports activities.
However, in consultation with the attending physician, sedentary work, such as in the office, is already possible in the first few weeks after the operation.
The developing tissue undergoes a maturation process. Therefore, even if the patient is free of pain, they must not put their full weight on the knee at first.
After about six months, sports activities can be resumed to the usual extent.