Here you can find additional information and selected specialists and centers for the treatment of bowel cancer.
Here you can find additional information and selected specialists and centers for the treatment of bowel cancer.
Recommended specialists
Brief overview:
- What is colorectal cancer? Colorectal cancer is a malignant tumor disease that occurs in the intestine (large intestine, small intestine, or rectum). It is the second most common cancer in men and women in Germany.
- Development: In most cases, the disease develops from benign intestinal polyps that can become abnormal over time.
- Risk factors: Factors such as genetics, inflammatory bowel diseases, diabetes, and an unhealthy lifestyle facilitate the cancer’s development.
- Symptoms: Symptoms do not appear until the disease is far advanced and include blood in the stool, diarrhea and constipation, crampy abdominal pain, and others.
- Diagnosis: Examination of a stool sample can provide information about the presence of colorectal cancer. A physician can turn to a colonoscopy to reliably detect an existing tumor.
- Treatment: Only surgical removal of the tumor offers a chance of a cure. Chemotherapy afterwards can support the treatment. Radiotherapy is only used for rectal cancer.
Article overview
- Definition: What is colorectal cancer?
- Incidence of bowel cancer
- Development and causes of bowel cancer
- Symptoms of bowel cancer
- Diagnosis and prevention
- Treating colorectal cancer
- After bowel cancer surgery
- Information on chemotherapy for colorectal cancer
- Psycho-oncological therapy
- Chances of curing colorectal cancer
- Specialists for colorectal cancer
Definition: What is colorectal cancer?
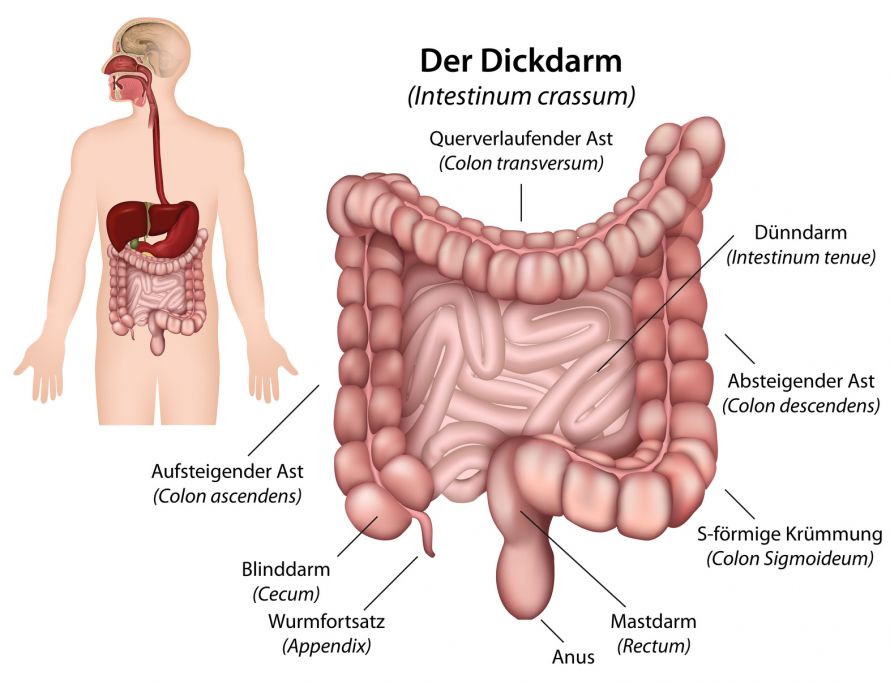
Bowel cancer refers to a malignant tumor in the large intestine, small intestine, or rectum. This tumor is caused by benign cells developing into malignant cells of the intestinal mucosa. In most cases, tumors develop in the colon or rectum. Tumors in the small intestine are extremely rare.
Doctors divide bowel cancer into the following technical terms:
- Colon carcinoma refers to a tumor of the colon. Colon surgery treats this form of bowel cancer.
- Rectal carcinoma refers to cancer of the rectum, where, the tumor is located in the last part of the intestine.
- Colorectal cancer refers to tumors in the colon and rectum.
Incidence of bowel cancer
Bowel cancer is the second most common cancer in Germany for both men and women (Robert Koch Institute 2006).
In Germany, approximately 73,000 people develop colorectal cancer each year and approximately 28,000 people die from it.
Statistically, 6 out of every 100 people in Germany will develop colorectal cancer during their lifetime, i.e., one in seventeen of us.
Development and causes of bowel cancer
As a rule, colorectal cancer develops from benign intestinal polyps. The degeneration of a benign intestinal polyp (adenoma) into malignant cancer (carcinoma) takes many years (adenoma-carcinoma sequence).
The degeneration is due to many successive gene changes (mutations) in the mucosal cells of the intestinal wall. These ultimately lead to loss of control over the cells’ growth, allowing the cells to divide unhindered and spread malignantly.
The process of degeneration occurs in several steps:
The mucosal cells begin to push over each other locally, gradually forming a small growth called an adenoma. The most common manifestation of such adenoma is an intestinal polyp. A polyp grows as a visible protrusion into the intestinal space. It can thus be easily detected and, if necessary, removed during a colonoscopy.
Ablation of a polyp during a colonoscopy | © Ortenau Clinic, License: CC BY 3.0
If the polyp is not detected, the genetic changes in the cells accumulate until they eventually become malignant cancer cells. If at some point they begin to proliferate into the surrounding tissue, this is referred to as "invasive" tumor growth.
The tumor cells slowly advance throughout the intestinal wall. In addition, individual cells can detach and spread in blood or lymphatic fluid to other parts of the body. There they can form secondary tumors (metastases).
This entire process, from polyp to cancer, is estimated to take over 5-10 years. The risk of such degeneration increases with age; most colorectal cancer patients are over 50 years of age.
However, the gene alterations may also be inherited (about 20-30% of cases). As a result, bowel cancer can develop at a younger age. If there is a family history of colorectal cancer, special care is required.
Other factors that can alter genes and thus facilitate cancer development include
- Tobacco smoke,
- Increased alcohol consumption,
- Being overweight,
- An unhealthy lifestyle and diet (insufficient exercise or consumption of fruit and vegetables),
- Chronic inflammation (Crohn’s disease, ulcerative colitis),
- Various chemicals,
- Radiation, and
- UV rays.
There is also an increased risk of developing colorectal cancer as a result of certain other types of cancers. This includes, e.g., breast or ovarian cancer.
Symptoms of bowel cancer
In the early stages of colorectal cancer, there are usually no or very few symptoms. As the disease progresses, the following initial signs may become apparent:
- Changes in bowel habits (alternating between constipation and diarrhea, changes in the stool’s consistency, color, odor, or frequent bowel movements)
- Blood in the stool
The detection of blood in the stool does not necessarily mean colorectal cancer. Other diseases, such as
- Hemorrhoids,
- Polyps, or
- Inflammation
are much more likely. Nevertheless, a diagnosis should always be conducted in these cases!
Other warning signs are
- A sudden decline in performance,
- Weight loss,
- Night sweats, and
- Fever.
However, such symptoms are by no means evidence of bowel cancer and also occur as a result of other diseases. Therefore, a precise diagnosis is recommended.
Diagnosis and prevention
The chances of curing colorectal cancer are better the earlier it is detected and treated. Regular screening can almost completely prevent and cure colorectal cancer. The colorectal cancer screening program offered by the statutory health insurers can and should be taken advantage of by anyone over the age of 50. Until the age of 55, you are entitled to one palpation of the rectum and one test for hidden blood in the stool per year.
After your 55th birthday, an additional colonoscopy is offered as a preventive check-up, even if no symptoms are present. If there is a family history of bowel cancer, a colonoscopy may need to be performed earlier because colorectal cancer has a very good prognosis and can be completely cured if detected early.

If detected early, colorectal cancer can be easily treated. Prevention is therefore very important! © Wolfilser | AdobeStock
Examination methods for the prevention or detection of colorectal cancer
First, the doctor performs a palpation examination of the rectum (digital rectal examination). In the process, the rectum, sphincter muscle, and the prostate are felt and assessed. Any abnormal findings must be clarified using a colonoscopy.
If necessary, further medical examinations will follow. The goal is
- To determine whether colorectal cancer is actually present (tumor detection),
- And if detected, determine how advanced it is (tumor staging).
In a detailed discussion, the doctor asks about the current symptoms, comorbidities, and risk factors.
Test for hidden blood in the stool (fecal occult blood test, stool guaiac test)
The rectum, sphincter, and prostate can be palpated and assessed with the finger. Any abnormal findings must be clarified using a colonoscopy.
Test for hidden blood in the stool (fecal occult blood test, stool guaiac test)
Three consecutive stool samples are tested in the laboratory for blood invisible to the naked eye. If blood is detected in the stool, this must be followed by a colonoscopy for further clarification.
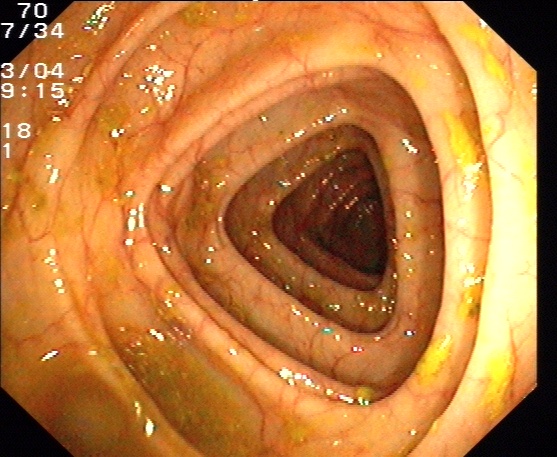
Colonoscopy
Only a colonoscopy, in conjunction with the removal of a tissue sample, can reliably detect colorectal cancer. Furthermore, the physician can detect intestinal polyps as possible precancerous lesions and remove them immediately.
Depending on the section of the intestine examined and the endoscope (camera and light instrument), colonoscopies can be further subdivided into:
- Colonoscopy (flexible endoscopy of the entire colon)
- Sigmoidoscopy (flexible endoscopy of the lower colon and rectum)
- Rectoscopy (rigid endoscopy of the rectum up to approx. 15-20cm)
Colonoscopy with normal findings | License: CC-BY-SA-3.0
X-ray diagnostics, CT scans, and MRI
These radiological procedures are not part of routine screenings but may be useful for specific issues. With a computed tomography scan (CT) or magnetic resonance imaging (MRI), layer images are taken of the inside of the body. These are further processed with special computer programs to produce a three-dimensional view of the inside of the intestine.
In addition to evaluating the general condition of the heart and lungs, X-rays of the lungs are used to search for possible colorectal cancer metastases in the lungs.
CT scans can be used to image not only the tumor itself, but also possible lymph node enlargements or metastases.
MRI uses alternating magnetic fields instead of X-rays. This technique allows the most accurate visualization of the spread extent and anatomy of a tumor, which is important for planning the surgery, e.g., for rectal cancer.
As with CT scans, enlarged lymph nodes or other organ metastases (especially in the liver) can be easily seen using MRIs.
X-ray examination (colon contrast enema)
In a colon examination with a contrast enema, the colon is filled with a contrast medium through the anus and shown on X-rays. However, inflammation and smaller polyps are more difficult to assess than with a colonoscopy. In addition, there is radiation exposure and the limited applicability of CT/MRI for patients with metal implants, pacemakers, or claustrophobia.
Ultrasound examination of the abdomen
An ultrasound (sonography) is a simple and risk-free examination method to show internal organs such as the liver, kidneys, or spleen.
Ultrasound examination of the abdomen is used to determine whether colorectal cancer metastases are present in other abdominal organs (e.g., liver).

Ultrasound is one of the imaging methods used in cancer diagnostics © auremar | AdobeStock
Blood tests, including tumor markers (CEA)
The amount of so-called tumor markers can be determined by means of blood tests. Tumor markers are substances that are increasingly produced by tumor cells but can also be found in healthy individuals.
A negative or normal tumor marker does not rule out cancer, nor does an elevated tumor marker prove it.
These levels are therefore mainly used to monitor the progression of the disease. An increase in the values would indicate a recurrence of the disease after tumor surgery.
The most important tumor marker for colorectal cancer is CEA (carcinoembryonic antigen).
Positron emission tomography (PET)
Cancer cells grow faster and therefore consume more energy and sugar than normal cells. This can be made visible with a positron emission tomography scan.
This is done by injecting a marked glucose that is taken up more by active cancer cells than by normal cells. The differences in the distribution of the marked glucose are then made visible in a special examination image.
A PET scan is not part of a routine examination for colorectal cancer, but is only used to answer specific questions. These include, e.g.,
- The response to chemotherapy or radiotherapy or
- A recurrence diagnosis.
At the same time, the results of the exam can be used to assess the risk of performing surgery (operability). This includes a thorough check of the functioning of vital organs, such as the heart and lungs.
Treating colorectal cancer
Surgical removal of the tumor is crucial for treating colorectal cancer and usually the only chance for making a complete recovery.
In general, however, healing can only occur if there has been no spread of tumor cells to other organs. Even in these cases, a cure is only possible in certain constellations nowadays.
Therefore, a precise evaluation of the disease’s extent (staging) must be performed before any surgery.
Colon carcinoma (cancer of the large intestine)
If colon carcinoma is diagnosed, surgery is performed as soon as possible after diagnosis and staging. The patient can only be cured if the tumor is completely removed.
To ensure this, the removed tumor is further examined and assessed by a pathologist after surgery. During the assessment, both the surgical margins of the specimen and the lymph nodes removed with it are checked.
Depending on the result, an additional chemotherapy may be necessary.
© bilderzwerg / Fotolia
Rectal carcinoma (cancer of the rectum)
In the case of rectal carcinoma, the first step after diagnosis is to clarify the exact size and invasion depth of the tumor.
For smaller tumors, immediate surgical removal of the tumor is recommended. For large tumors, pretreatment with chemotherapy and radiotherapy (or radiotherapy alone) is usually administered first to shrink the tumor.
This serves to simplify and reduce the risk of surgery and lowers the risk of tumor recurrence after surgery.

Medical linear accelerator for oncological radiotherapy © Thomas Hecker / Fotolia
Irradiation requires extremely precise planning. It is done on an outpatient basis for a few minutes a day, five days a week, for about a 5-week period. Again, there are side effects, including
- Diarrhea,
- Skin irritation (dryness, redness),
- occasional skin discoloration, and
- Hardening of the subcutaneous fatty tissue.
Whether additional chemotherapy is still necessary after surgery depends on various histopathological criteria.
However, radiotherapy (usually in combination with chemotherapy) is used only for rectal cancer. Before surgery (neoadjuvant) it is used to reduce the size of the tumor, while after surgery (adjuvant) it is used to prevent recurrences.
What information does the pathological examination of the surgical specimen provide?
After the operation, the pathologist's work begins. They examine the fine tissue of surgical specimens. Here, both the specimen and all removed lymph nodes are cut into extremely thin layers. This is followed by treatment with special stains that make it easier to identify tumor tissue.
Only these examinations can determine
- The exact size of the tumor,
- The depth of invasion, and
- The degree of differentiation.
In addition, the pathologist will check the surgical margins to make sure the tumor has been completely removed. As a rule, they attend the surgery and can thus instruct the surgeon to remove further tissue if necessary.
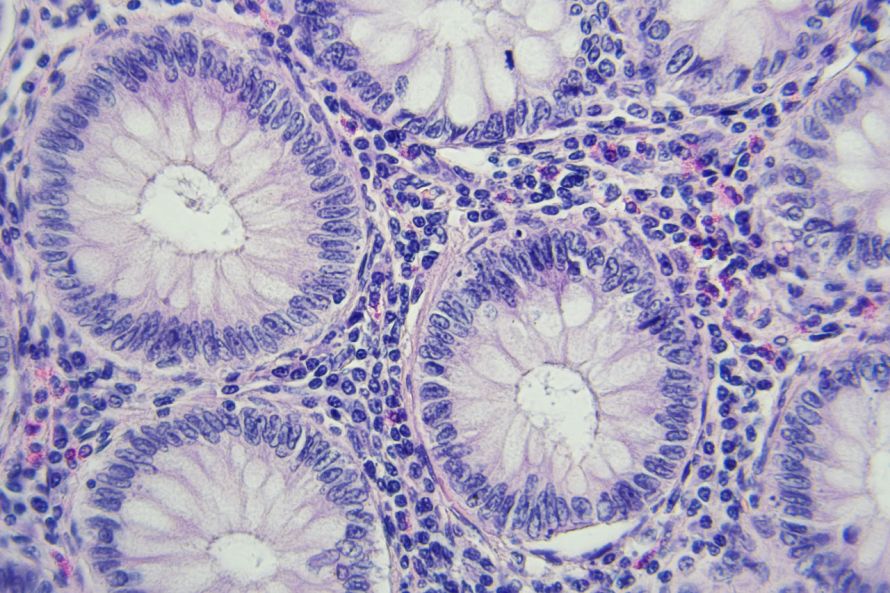
Tissue of the intestine at 400x magnification. Here, the pathologist can directly detect cancer cells © lukszczepanski | AdobeStock
Tumor classification
Important information can be obtained by processing the surgical specimen. This allows an accurate classification of the tumor.
This classification is called the TNM staging system. It reflects the individual extent of tumor spread for each patient. This is crucial for further treatment. In the TNM classification, three points are assessed as follows:
- T= tumor: Used to assess the depth of the invasion and the extent of tumor spread in individual bowel sections (T1 to T4)
- N= nodus (lymph nodes): Used to assess regional lymph node metastases (N0=none, N1=few to N2=numerous). Lymph node metastases are generally associated with a worse prognosis for the patient, therefore subsequent chemotherapy is recommended from stage N1.
- M= metastases: Used to evaluate distant metastases in other organs. The M stage is divided into M0 (=no metastases) or M1 (=metastases).
Tumor stage
Based on the tumor findings and the resulting TNM classification, the tumor is classified according to UICC criteria. A distinction is made between four stages, I-IV:
- Stage I: T1 or T2 N0 M0
- Stage II: T3 or T4 N0 M0
- Stage III: any T N1 or N2 M0 (lymph node metastases present)
- Stage IV: any T any N M1 (distant metastases present)
In addition, the "grading" is also assessed, which indicates the differentiation of the tumor. The degree of differentiation describes how similar the tumor tissue still is to the original intestinal tissue. The more the tissue has degenerated, the more aggressive the cancer:
- G1=well differentiated,
- G2=moderately differentiated, and
- G3=poorly differentiated.
Another important factor for prognosis and therapy is the R classification. It describes whether a residual tumor has remained in the body (residual tumor status).
For this classification, metastases remaining in the body and the surgical margins of the surgical specimen are assessed. The greater the distance between the surgical margins and the tumor is, the better the prognosis for the patient:
- R0= no tumor visible on the fine tissue
- R1 = fine tissue shows evidence of a residual tumor
- R2 = residual tumor or metastases visible to the naked eye.
After bowel cancer surgery
In tumor stages III and IV, additional recurrence or metastasis therapy is considered after the colorectal cancer surgery. Follow-up care for tumors is planned and organized with the involvement of all participating physicians. The prerequisites for this are
- A complete colonoscopy before or as soon as possible after bowel surgery, and
- An assessment of the patient's general condition.
Once all the findings are complete, it can be assessed whether and how often follow-up care for tumors is indicated on a case-by-case basis.
The goal of follow-up care is to detect as early as possible if
- The tumor starts to grow again (recurrence), or
- Secondary tumors form (metastases).
The risk of this is highest in the first two years after the surgery. Regular checks are therefore essential. After two years, the risk of recurrence continues to decrease over time. The intervals between checks can therefore be increased further and further:
- For colon cancer, checks should be conducted every 6 months for the first 3 years, and annually for the 4th and 5th years.
- On the other hand, 3-month intervals are recommended in the first year following rectal cancer.
After 5 years, colorectal cancer follow-up care is usually no longer necessary.
What does follow-up care for tumors in colorectal cancer entail?
Basic follow-up care includes
- A medical interview,
- A physical exam,
- Checking the laboratory parameters in the blood,
- Determining the levels of the tumor marker CEA,
- An ultrasound examination of the abdominal cavity, and
- An X-ray of the lungs.
Another integral part of follow-up care is undergoing a colonoscopy.
For colon cancer, it is recommended that a colonoscopy be performed once a year. A rectoscopy is recommended for rectal cancer, especially at the beginning of every follow-up examination.
CT scans are not routinely used for colorectal cancer follow-up care. However, they can be helpful to record the initial status after surgery to quickly detect even the smallest change.
Diet following surgery for bowel cancer
Following colorectal cancer surgery, the patient can specifically influence the following through their diet:
- Stool consistency,
- Flatulence, and
- Their general well-being.
Nevertheless, there are neither binding dietary recommendations nor blanket prohibitions.
Avoiding certain foods
The basis of nutritional therapy is an "adapted balanced diet", i.e., the avoidance of foods and beverages that experience has shown frequently lead to intolerances. These include
- Legumes,
- Mushrooms,
- Cabbage vegetables,
- Raw onions,
- Garlic,
- Leeks,
- Fried food,
- Wholewheat bread with whole grains,
- Freshly baked bread,
- Hard boiled eggs,
- Acidic foods,
- Overcooked food,
- Smoked food,
- Spicy food,
- Food and drinks that are too hot or too cold,
- Carbonated drinks, and
- Unripe fruit.
It is recommended to keep a meal and symptom diary for an individual assessment of food tolerances.
Dietary recommendations
During colorectal cancer surgery, an artificial bowel outlet is sometimes built into the small intestine (ileostomy or jejunostomy). In this case, the colon cannot carry out its normal functions, resulting in decreased reabsorption of water and electrolytes. This results in thin, mushy stools and increased stool frequency.
For the affected person, it is important to know that any intake of food or drink leads to bowel discharge. Eating and drinking slowly and chewing thoroughly can be very helpful in such cases.
In the long term, it is recommended to change one’s diet to the Mediterranean diet, which not only prevents heart disease and being overweight, but also certain forms of cancer. The Mediterranean diet includes
- The daily and abundant consumption of fruits, vegetables, and salads,
- A preference for vegetable fats, such as rapeseed oil, olive oil, or soybean oil,
- A reduction of fat (dairy products in moderation, infrequent consumption of red meat and sausages),
- The frequent consumption of fish (2-3 servings per week), and
- Moderate consumption of alcohol, if possible.
In addition, the Mediterranean diet also includes
- A healthy lifestyle,
- Rest and time to eat, and
- Regular physical exercise.

The Mediterranean diet helps support the body after bowel cancer treatment © aamulya | AdobeStock
Do I need chemotherapy after bowel cancer surgery?
If tumors are detected in the lymph nodes, postoperative (adjuvant) chemotherapy is recommended.
In this case, although the tumor itself was completely removed, there still is a risk (up to 50%) that individual cancer cells have already settled in other parts of the body. These cannot be detected with today's methods.
Large-scale studies have shown that prophylactic (adjuvant) chemotherapy significantly reduces the risk of relapse.
Even in lower tumor stages, other indications for adjuvant chemotherapy would be if
- The tumor ruptured during the colorectal cancer surgery,
- The tumor has poor cell differentiation (G3), or
- Fewer than 12 lymph nodes were removed during surgery.
In these cases, experts must decide on an individual basis whether chemotherapy is indicated or not.
If the colorectal cancer has been detected at a late stage, it has already metastasized. In this case, so-called palliative chemotherapy is indicated. A cure is then usually no longer possible. The therapeutic goal is then to improve the quality of life and prolong that life.
In some cases, chemotherapy can shrink colorectal cancer metastases to the point where they can be surgically removed.
Information on chemotherapy for colorectal cancer
Cells that divide rapidly, similar to cancer cells, are the target of chemotherapy. Unfortunately, this also affects healthy tissue with a high division rate, such as hair cells. The blood distributes the drugs, also called cytostatics, throughout the body. Therefore this treatment is referred to as a "systemic therapy."
What medications are used?
Nowadays there are a wide variety of drugs available. Oncologists select and combine them depending on the patient's individual case.
Usually, several drugs are used according to a proven fixed regimen (e.g., FOLFOX regimen). Chemotherapy can be performed on an outpatient basis provided there are no health problems suggesting otherwise. Implantation of a venous port catheter may be required for administering the medications. This makes treatment easier and more comfortable for the colorectal cancer patient.
Adjuvant chemotherapy usually lasts six months. However, the duration of treatment may be prolonged in the metastatic stage depending on the response to therapy.
In these cases, so-called antibodies (e.g., cetuximab, bevacizumab) can be used in addition to the classic cytostatics. Antibodies bind to and block specific surface structures on cancer cells that are important for tumor growth.
However, antibodies aren’t significant (so far) in regular "adjuvant" therapy.
What side effects can occur with chemotherapy?
The possibility of side effects occurring during chemotherapy is based on the fact that rapidly dividing healthy cells are also killed. However, they do not necessarily occur.
This includes, e.g., bone marrow, in which the various blood cells are formed. As a result, the following symptoms may occur over the course of therapy
- Anemia,
- Hemorrhaging, and
- Infections.
The white blood cells are critical for the body’s defense against infections. They absolutely require regular monitoring (blood count) during chemotherapy. If their number drops too much, the therapy must be interrupted for a recovery period.
The tissue of the digestive tract is also one of the rapidly dividing ones and chemotherapy can cause various side effects. These include
- Nausea,
- Vomiting,
- Loss of appetite,
- Taste disorders, and
- Diarrhea.
Fortunately, there are some very efficient drugs (e.g., antiemetics) against these side effects.

In some cases, chemotherapy is used for colorectal cancer © Elnur | AdobeStock
Another possible side effect of some cytostatic drugs is hair loss. However, complete hair loss is not expected with the drug combinations used to treat colorectal cancer.
In any case, hair grows back after the end of treatment. The other side effects mentioned above also disappear following the termination of treatment.
In terms of the above-mentioned antibodies, there are generally few side effects to worry about. Since proteins are involved, allergic reactions may occur rarely (e.g., an acne-like rash with cetuximab).
In general, your treating oncologist should inform you about any expected side effects corresponding to the therapy regimen. If necessary, they will treat the effects with additional medication.
Psycho-oncological therapy
Research has shown that there are no general factors that improve or worsen our quality of life. The term quality of life means one’s personal experience with cancer. This includes sensations and discomfort in mental, physical, and social life.
Therefore, there are big differences between different people in how they deal with the disease. Each patient processes the stresses that the disease or treatment may cause differently.
Many of these stresses are temporary, but they can also be persistent and require psychological treatment.
During hospital treatment, patients are often preoccupied by fear of the operation. It is important to ask as much as you want to know and understand in your discussions with your treating physician. Your own concerns and worries should also be brought up. After being discharged from the hospital, patients are often overwhelmed by the many requirements.
Many cancer patients’ main concern is that the disease may recur or spread ("progression anxiety"). This concern is normal and appropriate; however, it can also get out of control.
In this situation, it can be helpful to talk about it and confront the fear. The importance of mental illness processing is increasingly recognized. As a result, there are a variety of appropriate support options available today in psycho-oncology.
Chances of curing colorectal cancer
The overall prognosis for colorectal cancer depends primarily on the extent to which the tumor could be removed. The earlier the tumor is detected and removed, the better the chances of recovery.
Due to improved preventative examinations, over 50% of cases are curable today. However, if colorectal cancer metastases are already present in other organs or lymph nodes at the time of diagnosis, the prognosis is significantly worse.
Specialists for colorectal cancer
Specialists for colorectal cancer usually come from the departments of abdominal surgery and/or gastroenterology. These two departments collaborate on treating colorectal cancer, especially in the fields of
- Oncology,
- Radiotherapy,
- Radiology, and
- Pathology.
In addition to these medical fields,
- Pain and physiotherapy,
- Specialized oncological care, and
- So-called supportive therapy
also play a major role. Supportive therapy includes, but is not limited to
- Pastoral care,
- Psycho-oncology,
- Social service,
- Nutritional counseling, and
- Self-help groups.
The latter support patients affected by colorectal cancer and their relatives throughout the treatment process.